
The Mystery & Magic Of The Pelvic Floor Muscles
No one wants to experience bladder or bowel incontinence, rushing to the toilet or difficulties emptying, prolapse, pelvic pain or pain with sex. Unfortunately, these issues are common across all genders and substantially impact physical, emotional, social and financial health and wellbeing. There is often associated stigma, leading to people suffering in silence, thinking it is normal or that nothing can be done to help.
The Pelvic Floor Muscles (PFM) can be part of the problem and part of the solution for each of these issues. For such a crucial muscle involved in important bodily functions, it is surprising that the PFM are often forgotten. This is partly due to them being ‘out of sight, out of mind’ and so learning where they are, how they work and what exercises are appropriate can be lifechanging. We hope to reduce the mystery and reveal the magic of this amazing muscle!
Where Are The Pelvic Floor Muscles?
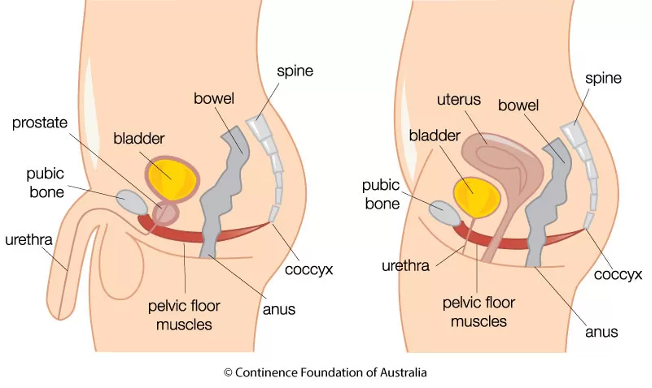
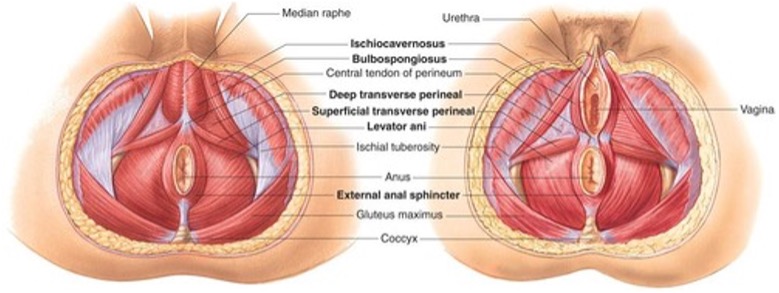
The PFM are a layered (superficial and deep) group of muscles that span the base of the pelvis, like a hammock. They attach at the front of the pelvis to the pubic bone and extend back to attach to the tailbone (coccyx) and fan out sideways to the pelvic sit bones (ischial tuberosities). The urethra (the tube from the bladder), the vagina (in women) and the rectum and anus (the back passage) all pass through the pelvic floor.

What is the Role of the Pelvic Floor Muscles?
The role of the PFM is to support the pelvic organs (bladder, bowel and uterus in women), helping to maintain the position of these organs in the pelvis. They play a part in providing bladder and bowel control and they relax to allow urination and bowel emptying.
The PFM play a role in sexual function, contributing to sensation, arousal and orgasm. They need to relax to allow vaginal or anal penetration and assist in gaining and maintaining erection.
The PFM is a clever and complex muscle; they function at rest, when they contract (switch on) and when they relax (switch off). They also work alongside other muscles in the trunk and pelvis eg the abdominal and back muscles and the diaphragm. The PFM is quite unique in terms of its protective nature, helping to keep the precious contents of the pelvis safe – the bladder and bowel, required for survival and the reproductive organs and genitals, vital for procreation, pleasure and intimacy. You can see why they are intricately connected to our brain and nervous system.
How To Correctly Contract The Pelvic Floor Muscles
 A correct pelvic floor contraction should incorporate a squeezing and lifting action, that starts around the back passage and lifts forwards and upwards towards the pubic bone1. The upper abdominals, gluteal and inner thigh muscles should remain completely relaxed. It is important that breathing is relaxed and easy whilst maintaining a PFM contraction. The PFM should be able to return to a relaxed resting state after a contraction.
A correct pelvic floor contraction should incorporate a squeezing and lifting action, that starts around the back passage and lifts forwards and upwards towards the pubic bone1. The upper abdominals, gluteal and inner thigh muscles should remain completely relaxed. It is important that breathing is relaxed and easy whilst maintaining a PFM contraction. The PFM should be able to return to a relaxed resting state after a contraction. One of the challenges of doing PFM exercises is that it’s difficult for people to know if they are achieving a correct contraction and relaxation. In fact, research has shown that most people, when given verbal or written instructions will perform an incorrect or ineffective contraction, some even bearing down and potentially making their symptoms worse2. We commonly see people who have previously done PFM exercises eg in a Pilates class and on assessment discover that they are not correctly contracting the muscle. This can occur for a number of reasons.
Problems With Pelvic Floor Muscle Function:
Just like any other muscle in the body, the PFM can have1:
- Increased tension at rest
- Decreased tension at rest
- Decreased strength / weakness
- Decreased endurance
- Incomplete or delayed relaxation
- Tenderness or sensitivity to touch
- Poor co-ordination. For example:
- Contracting when it should be relaxing
- Relaxing when it should be contracting
- Incorrect timing of contraction
- Incorrect isolation of contraction - Poor attachments to the bones (via connective tissues)
What can lead to PFM function problems3?
- Pregnancy & childbirth
- Constipation & straining
- Ageing & menopause
- Chronic cough
- Heavy lifting
- Strenuous sports
- Neurological conditions
- Over-training of core / abdominal muscles
- Holding tension in the PFM due to stress, threat, pain, movement issues or injury elsewhere in the body
Problems with the PFM can be part of the following conditions3 (to name a few):
- Urinary incontinence
- Stress Incontinence
- Urgency & Urge Incontinence
- Faecal Incontinence - Bowel Urgency
- Difficulties emptying bladder and bowel
- Pelvic Organ Prolapse
- Sexual Pain in women
- Sexual & Pelvic Pain in men
- Persistent Pelvic Pain
- Sexual Dysfunction
- Erectile dysfunction
Pelvic Floor Muscle Training: A Solution For PFM Problems
A PFM training program is most effective when based on individual assessment. This assessment should be performed by a Pelvic Health Physiotherapist who has specific post-graduate training. The physical assessment is just one part of a comprehensive, whole person assessment process.
Always with fully informed consent and consideration of past experiences, the assessment involves a combination of vaginal or rectal examination, transperineal ultrasound, visual or external assessment. This helps to answer questions such as;
- Does the PFM need to be stronger?
- Does the PFM need longer endurance?
- Does the PFM need to coordinate with activity eg be able to contract with coughing
- Does the PFM need to more effectively relax?
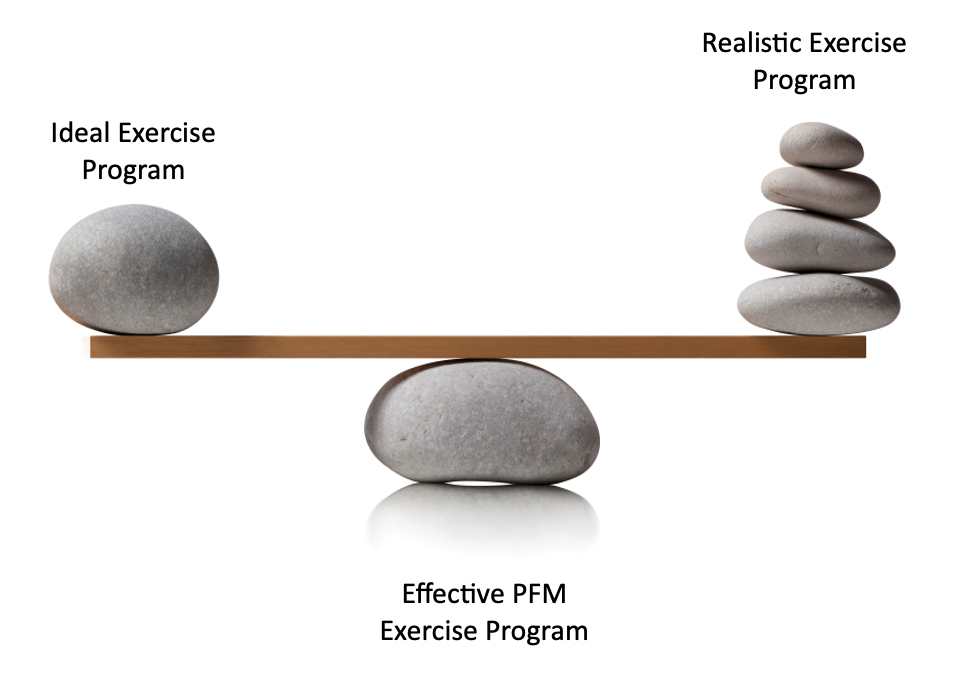
This information is considered along with research recommendations, muscle training principles, the patient’s symptoms and lifestyle and an individualised exercise program is designed. Effective PFM training programs often involve performing a few sets per day which leads to a balancing act between what exercise program is ideal with what is realistic.
Do PFM Training Programs Work?
There is a mountain of research and evidence that proves how effective PFM training can be for pelvic health conditions.
- PFM training should be offered, as first line therapy, to all women with stress, urge or mixed urinary incontinence3
- Positive results of PFM training can be maintained in the long term (one year post treatment)3,4
- PFM training should be offered, as first line therapy, to all women with Pelvic Organ Prolapse3
- PFM training in pregnancy can prevent Stress Urinary Incontinence3
- Supervised PFM training postnatally is more effective than a control group (i.e. people doing PFM training without a physio advising them)
- PFM training reduces prevalence of urinary incontinence in young athletes and postmenopausal women2,3
- Commencing PFM training pre-operatively improves time to continence after Prostate Cancer surgery4
- Research shows PFM training prescribed, supported and progressed by a trained pelvic health physiotherapist is more effective than independent PFM training2,3
Overall, international guidelines strongly recommend an individual assessment and training program. This ensures a correct contraction, specific training needs are met, progression and modification and ultimately the best possible outcome.
Reduce the Mystery and Discover The Magic of Your PFM With Us
We hope everyone is curious to uncover the mystery and discover the magic of their pelvic floor muscles! Our postgraduate trained Pelvic Health Physiotherapists look forward to supporting you to achieve your pelvic health goals so you can live your best life.
References
1 Frawley H, Shelly B, Morin M, Bernard S, Bø K, Digesu GA et al. m An International continence society (ICS) report on the terminology for pelvic floor muscle assessment Neurourol Urodyn. 2021;1–44.
2 Bo, K. Physiotherapy management of urinary incontinence in females. Journal of Physiotherapy 66 (2020) 147–154
3 Dumoulin C, Adewuyi T, Booth J, Bradley C, Burgio B, Hagen S, et al. Adult conservative management. In: Cardozo L, Rovner E, Wagg A, Wein A and Abrams P eds. Incontinence. 7th Ed. 2023:795-1038
4 Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H et al. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. Urologic Oncology, Seminars and Original Investigations. 2020;38: 354−371
September 2024




