Vulva & Sexual Pain
Do you have pain or sensitivity in your vulva or vagina?
Do you have difficulty inserting a tampon or with a vaginal examination?
Does it hurt to wear tight clothing?
Have you been diagnosed with vulvodynia or vaginismus?
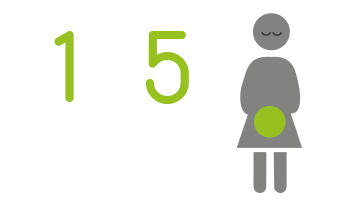
One in five women experience vulval pain or painful sex, but most are too embarrassed to talk with their doctor or confide in a friend. These symptoms are often highly distressing, leading to women withdrawing socially, avoiding relationships and intimacy, and reducing self-esteem. The two most common conditions associated with vulval or sexual pain are vaginismus and vulvodynia.
What are Vaginismus and Vulvodynia?
Vaginismus is a condition that involves spasm of the pelvic floor muscles, tightening the vaginal opening and making it painful (or impossible) for anything to enter, such as a tampon, a penis, or during an internal vaginal examination. Vulvodynia is a condition where there is pain, burning or discomfort in the vulva (skin outside the vagina) which cannot be linked to a specific cause. There are two main subtypes of vulvodynia, provoked vulvodynia and generalised vulvodynia.
- Provoked vulvodynia is when symptoms occur with touch or pressure to the vulva with activities that should not normally be painful, such as inserting a tampon or sexual intercourse.
- Generalised vulvodynia is vulval pain which occurs spontaneously and can be relatively constant. These symptoms are often exacerbated by touch or pressure to the vulva, such as wearing tight clothing.
Common Symptoms:
Vulval or vaginal pain may be there all the time, or it may only occur with activities like sitting, wearing tight pants, vulval touch, or vaginal penetration, such as using a tampon or having sex. Some examples of common symptoms experienced:
• Difficulty with vaginal penetration, feeling ‘too tight’ or ‘blocked’
• Painful sex, which can be felt deep in the vagina or close to the vaginal entrance
• Pain or inability to use tampons or have a pap smear / cervical screening test
• Pain or burning in the vagina or vulva with touch, sitting, or tight clothing
• Pain with arousal
• Low libido
• Fear and worry about sex or using a tampon
What Causes Vulval & Sexual Pain:
Vulval and sexual pain can occur for many different reasons, but some of the more common causes are:
• Skin conditions of the vulva, such as Eczema, Dermatitis and Lichen Sclerosus, infections, such as Thrush and Sexually Transmitted Infections (STIs)
• Conditions such as Vulvodynia or Vaginismus
• Other medical conditions such as Endometriosis, Adenomyosis, Interstitial Cystitis, and Irritable Bowel Syndrome.
• Changes during Menopause, including the condition Genitourinary Symptoms of Menopause (GSM)
• Emotional factors such as anxiety, stress, low mood and relationship problems
• Things that have occurred in your past, such as a history of trauma or abuse
How We Can Help:
Our experienced Physiotherapists understand this complex problem and will work with you to improve your quality of life. We take a wholistic approach addressing all aspects that may be contributing to your pain. Your physiotherapist will take a detailed history to work out what is causing your pain. They will help you understand your pain and how your muscles, nerves, thoughts and feelings and the world around you are contributing. We know how to reduce pelvic muscle tension and pain and restore enjoyable intimacy. We work closely with you, your referring doctor and other health professionals to achieve your goals.
What To Expect:
Our caring physios are invested in your overall wellbeing, empowering you to live your best life. During your treatment with us you can expect:
• Time spent hearing and exploring your story, understanding your unique body, mind and lifestyle factors and establishing goals with you
• A thorough physical assessment, which may include an internal vaginal examination (if and when you are ready)
• A detailed explanation of what is causing your pain, helping you to make sense of your pain and what we can do to help
• Design of a treatment program tailored to your individual needs and goals
• Exercises for your pelvic floor muscles
• Education about intimacy, arousal and libido and how to integrate relaxation into an intimate setting
• Education about the science of pain, to help you understand the relationship between your pain, nervous system, and physical and emotional health
• Techniques to help desensitise the muscles and skin at the vaginal entrance, to help your body learn that touch is safe
• Advice on lifestyle factors including general exercise, sleep, diet and stress management
To learn more, you might be interested in our blog, Painful Sex Is Not Ok
Did You Know