
Get Control & Stop Leaking When You Cough, Sneeze or Exercise
Urinary Leakage is Common and Impactful
In Australia, over 7.2 million Australians are affected by urinary leakage or incontinence – 2.4 million men and 4.8 million women. That’s a staggering 1 in 3 women and 1 in 10 men having difficulty controlling their bladder.
The impact on individuals can be significant; withdrawal from exercise and other pleasurable activities, avoidance of social situations and intimacy, embarrassment of wetting clothes and worry around finding toilets. There are also significant financial costs to the individual (eg using pads) and to society with a recently released Deloitte Access Economics report revealing the cost of incontinence to Australia in 2023 was $100.4 Billion.1
Despite its prevalence and impact, incontinence remains under recognised and under reported, with most people affected putting up with it for years, believing it is normal and there isn’t anything that can help. The good news is, the majority of people can be treated, better managed or even cured.
Stress Urinary Incontinence (SUI)
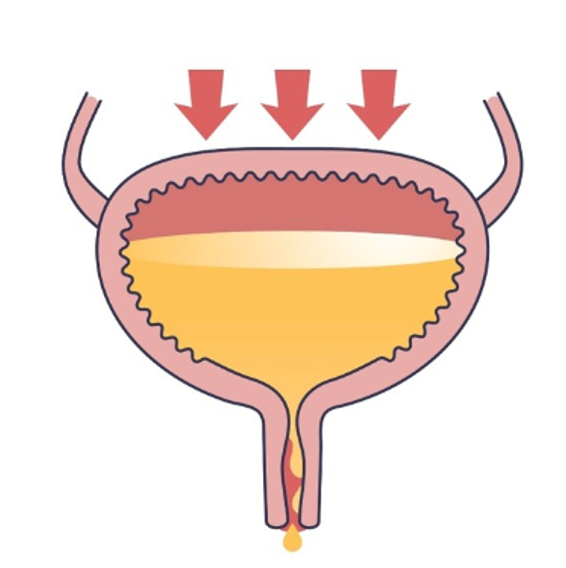
The most common type of urine leakage is Stress Urinary Incontinence (SUI). Confusingly the term “stress” doesn’t refer to emotional stress but pressure created in the abdominal cavity. SUI occurs during activities or tasks that place a downward pressure or force on the bladder, causing urine to escape out accidentally through the urethra - the tube from the bladder that urine passes through. If the pressure on the bladder of the effort or exertion is greater than the support and closure of the urethra, leakage will occur.
Common activities that can trigger SUI type leakage include:
- Coughing
- Sneezing
- Jumping
- Changing position
- Walking
- Running
- Heavy lifting
- Weight & resistance training
- Laughing
The amount of urine loss can vary, from a drip to a spurt (most common) or even complete bladder loss (less common).
Why Does Stress Urinary Incontinence Occur?
Why SUI happens is not fully understood. There are currently two research-based theories regarding the underlying mechanism of SUI.2 A person with SUI may have one or both of these.
- Hypermobility of the urethra: Increased mobility of the tissues that support the bladder neck (area where the urethra joins the bladder) and the urethra (tube from the bladder that urine passes through).
- Urethral Sphincter weakness: Reduced function of the sphincter muscle that wraps around the urethra and the mucous membrane inside the urethra that helps provide closure. The weakness can exist at rest or during activities where increased closure pressure is required.
Risk Factors For SUI
There are many reasons why the above changes can occur, leading to SUI2:
- Pregnancy & childbirth; pregnancy and childbirth can lead to a stretching and weakening of the tissues that support the urethra and bladder, as well as damage to the nerves in the pelvis.
- Hormonal changes; reduced levels of oestrogen can impact the health of the mucous membrane of the urethra. For many women, problems with SUI start around the time that they notice peri-menopausal changes occurring.
- Surgery:
- Prostate Surgery
When part or all of the prostate is surgically removed, this can cause impairment to the structures and tissues that support the urethra and bladder neck. - Hysterectomy
Surgery to remove the uterus can lead to a change in tissue support. - Chronic respiratory disorders; over time, ongoing and repetitive coughing can weaken and stretch the tissues that support the urethra and bladder neck.
- Heavy lifting/high impact exercise; due to the increased pressure of the lifting or type of exercise on the bladder in people that do not have enough support of the urethra to counteract the pressure forces.
- Obesity; obesity is perhaps the most clearly established risk factor for UI in women. Overweight and obese people have more pressure on their bladder when they exert themselves
- Constipation & straining; prolonged straining on the toilet can stretch and weaken the muscles and nerves of the pelvic floor and the urethra, leading to reduced support.
- Pelvic Organ Prolapse; this occurs when any of the pelvic organs – the bladder, uterus or rectum moves down out of its normal position and bulges into the vagina. When this occurs, there can also lead to a reduction in support of the bladder and urethra.
- Ageing; leads to loss of mucosal support which can contribute to urethral sphincter weakness.
- Genetics: it is possible that people who inherit more elasticity in their tissues might be more prone to SUI, though further research is needed on this.
SUI Can Be Cured With Pelvic Health Physiotherapy!
The good news is that SUI can be successfully treated with the right advice and an individualised pelvic floor muscle (PFM) training program. Studies have shown an 84% cure rate of SUI for people participating in a physiotherapy led training program3. Pelvic floor muscle training is therefore recommended in international guidelines as the first line treatment to not only improve SUI, but to also prevent it4.
Research also has proven that getting the right advice from a Pelvic Health Physiotherapist with a PFM training program can lead to better and faster outcomes4,5.
Alongside pelvic floor muscle exercises, other treatment strategies for SUI may include5:
- Fluid intake advice
- Education and advice on good bladder habits
- General exercise and lifestyle modification advice
- Weight loss strategies
- Strategies on how to avoid straining on the toilet
- Vaginal pessaries to support a pelvic organ prolapse and the urethra
- Surgery, if at least 6 months of Physiotherapist led PFM training has been unsuccessful
At Women’s & Men’s Health Physiotherapy, we will explore your symptoms, hear your history, gather further relevant information, understand your goals, assess your pelvic floor muscles and help you make sense of why you have SUI. We then discuss all available treatment options and collaboratively develop an individualised program that includes a tailored pelvic floor muscle training program. We work with you to restore pelvic health and empower you to live your best life.
Stress Urinary Incontinence Success Stories:
Here we share 3 stories of people with SUI that represent patients we commonly see in our practice.
- Julie was worried about not being able to play with her grandchildren in the park.
- Chloe was frustrated about not being able to exercise without leaking after giving birth to her daughter.
- Robert wanted to get back on the golf course and catch up with his mates at the 19th hole.
Meet Julie, she is 58 years old and had 3 vaginal births in her early to mid 20’s. She experienced occasional leakage with coughing and sneezing during each pregnancy and for a short period after each baby. Since going through menopause, she noticed her urine leakage was slowly worsening. She started to wear a pad every day, leaking whenever she coughed, sneezed or lifted / ran after her grandchildren. It was having an impact on her confidence leaving the house as she was always wanting to know where the nearest toilet was so that she could empty her bladder ‘just in case’.
She told her GP about her concerns with her bladder, who referred her to WMHP. As part of her assessment, it was discovered that Julie had difficulty isolating her weak pelvic floor muscles (she was overusing her buttock muscles and holding her breath) and she also had difficulty coordinating a PFM contraction when she coughed or performed an activity that created pressure in her abdomen. She was taught how to contract her PFM correctly and started an individualised exercise program based on her specific strength, endurance and timing deficits. Julie had a review of her exercise program on an intermittent basis over the next few months, where her Physiotherapist provided feedback on her technique and progressed her home PFM program.
Over a six-month period, Julie experienced significant improvement in her bladder control. She reported recently having a cold and despite coughing frequently, was proud that she had could contract her pelvic floor before coughing and stay dry! Julie was no longer wearing a pad and could confidently lift and run after her grandchildren without leaking – or worrying about it!
Meet Chloe, she is 31 years old and loving being a new mum to her baby daughter, Ruby who was born via a caesarean. Chloe was keen to get back to exercise and when Ruby was 12 weeks old, she started going for a jog around the block and doing squats, deadlifts and upper body weights in her home gym. By the end of her jog, Chloe would leak small amounts with each step she took. She also started leaking when she did a deadlift. She’d heard some of the other mum’s in her mother’s group complain about the same thing, but she didn’t want to put up with it. Chloe had read about pelvic floor exercises and so she made an appointment to see a Pelvic Health Physiotherapist at WMHP.
Chloe’s Physio performed a thorough assessment, which included asking her about her bladder and bowel habits as well as assessing her pelvic floor muscles with a vaginal examination. Since giving birth she had been constipated, straining on the toilet every 2nd day to empty her bowels. Her Physio noted that Chloe was actually bearing down when she tried to contract her PFM. With visual feedback and education regarding correct technique, Chloe was able to learn how contract her PFM correctly but her muscles were very weak.
Chloe’s Physio prescribed an awareness and strengthening program for her pelvic floor muscles. She was also taught a more ideal way of sitting on the toilet to empty her bowels and was given advice to increase the amount of fruit and vegetables (particularly prunes and kiwi fruit) to help to soften her stools. Chloe benefited from having regular re-assessment and feedback on her pelvic floor exercises in the first 6 weeks so that she could improve her PFM technique and connection and confidence with the home program. Chloe and her Physio agreed on a graduated general exercise program that would allow Chloe to improve her fitness and general strength, without causing leakage. Over the next 3 months, Chloe’s PFM strength and function significantly improved and she started the Couch to 5km running program. She was delighted that she could progress her running and is now comfortably running 5km without leaking!
Meet Robert, he is 63 years old and had recently been diagnosed with Prostate Cancer. In consultation with his Urologist, he decided to undergo keyhole surgery to remove his prostate (Robotic Assisted Prostatectomy). He was told to expect urine leakage after surgery, caused by coughing, sneezing, bending over, lifting and standing up from a chair. His Urologist referred him to WMHP prior to his surgery, to learn where his pelvic floor muscles were (he never knew that they existed in men!) and how to exercise the muscles correctly.
Robert was shown how to contract and relax his pelvic floor with the use of ultrasound placed on the perineum, allowing him and his Physiotherapist to clearly see the muscles contracting and relaxing. He was also provided with education regarding good bladder and bowel habits and what to expect after surgery. He was diligent with his exercises prior to surgery and he continued them afterwards. His exercises were monitored and progressed by his pelvic health physiotherapist, who adjusted his exercise program based on what activities were causing leakage, and how his PFM function was progressing.
In the first few weeks after surgery, Robert was wearing 3-4 pull up pads per day to contain his urine loss. Over the next 6 months, Robert experienced gradual reduction in urine leakage. At 3 months was using 2 smaller pads, only leaking if he forgot to contract his pelvic floor when he changed position or swung his golf club. At 6 months, Robert was no longer wearing pads at home, only wearing a pad ‘just in case’ when playing golf. By 8 months, he was completely dry, no longer wearing a pad and improving his handicap!
If you, or someone you know is bothered by urine leakage, seek help from a Pelvic Health Physiotherapist at Women’s & Men’s Health Physiotherapy who can guide you with an individualised treatment plan to improve your bladder control.
References
2 Falah-Hassani K, Reeves J, Shiri R, Hickling D, McLean L. The pathophysiology of stress urinary incontinence: a systematic review and meta-analysis. International Urogynecology Journal (2021) 32:501–552 https://doi.org/10.1007/s00192-020-04622-9
3 Neumann P, Grimmer K, Grant R, Gill V. Physiotherapy for female stress urinary incontinence: a multicentre observational study. Australian and New Zealand Journal of Obstetrics and Gynaecology 2005; 45: 226–232
4 Dumoulin C, Adewuyi T, Booth J, Bradley C, Burgio B, Hagen S, et al. Adult conservative management. In: Cardozo L, Rovner E, Wagg A, Wein A and Abrams P eds. Incontinence. 7th Ed. 2023:795-1038
5 Bo, K. Physiotherapy management of urinary incontinence in females. Journal of Physiotherapy 66 (2020) 147–154
September 2024




