Rushing to the Toilet? You’re not alone!
Overactive bladder (OAB) is a common condition affecting up to 10-20% of men & women, affecting people of all ages, with most over the age of 40. It is under diagnosed and under treated because people incorrectly assume it is an inevitable part of ageing or nothing can be done to help.
The main symptom of OAB is urgency, which is a feeling of a sudden, strong desire to pass urine which is difficult to put off. People may also experience symptoms of:
Frequency – going to the toilet more often than normal
Urge urinary Incontinence – leakage of urine when rushing to the toilet
Nocturia – waking more than once overnight to pass urine.
These problems can lead to a loss of freedom with life literally revolving around the toilet with a constant fear of not making it. Waking at night can increase the risk of falling and lead to chronic tiredness.
Why Does Overactive Bladder Occur?
OAB is thought to be due to a combination of local bladder and central brain factors, including:
- Changes in the way the brain responds to messages from the bladder
- Weak or tight pelvic floor muscles
- Extra sensitive nerves in the bladder
- Poor bladder & fluid intake habits
- Hormonal changes
- Bladder problems eg recurrent UTI’s or poor emptying
- Enlarged prostate
- Neurological diseases eg Parkinson’s Disease or stroke
The Bladder & The Brain in OAB
The brain interprets messages from sensors (like an alarm sensor) in the bladder that detect pressure, stretch, chemicals, in conjunction with other information such as past experiences (eg previous accidents or near misses), worry, context and environment which contributes to the strength of the urge sensation.
The feeling of urge comes from the brain, not from the bladder
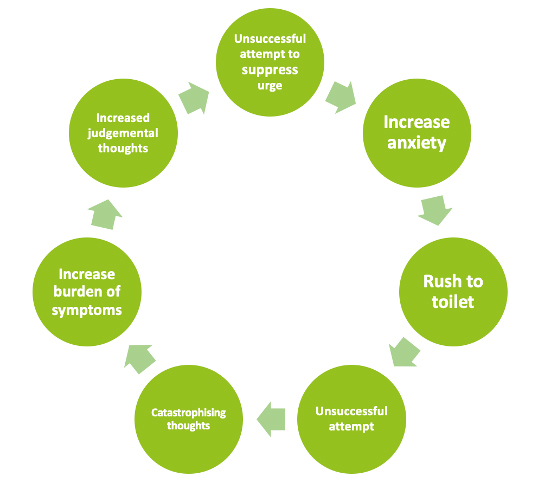
In OAB, the bladder messages can be interpreted by the brain as a threat, which may lead to a sense of anxiety and a fear of leakage, activating the “fight or flight” response. This can result in a misleading message telling the bladder to empty. Racing to the toilet with strong urgency leads to panic, worry which strengthens the negative urgency cycle.
What can be done about OAB?
The good news is that OAB can be successfully treated and symptoms can improve. International guidelines suggest that Pelvic Health Physiotherapy, including pelvic floor muscle training and bladder training, should be the first line treatment for OAB.
Pelvic Health Physiotherapy Assessment for OAB
- Thorough history: including understanding symptoms, when they started and the impact they are having on quality of life
- Rule out infection: a screening urine test can rule out a UTI and identify if further investigation is required
- Check bladder emptying: a bladder ultrasound performed in the physiotherapy clinic can assess if the bladder is emptying properly
- Bladder diary: a 2-3 day record of fluids, bladder volume and urgency provides valuable insight into bladder habits including the volume the bladder can hold, the context of when urgency occurs and the impact of fluid intake
- Pelvic floor muscle assessment: Weak pelvic floor muscles can contribute to reduced bladder support and control, whilst tense pelvic floor muscles can lead to more sensitivity in the bladder and nerves. An assessment may involve a vaginal examination (for women), a rectal examination (for men) or an ultrasound
- Bowel diary: identification of bowel issues can affect the bladder
- Lifestyle factors: exercise, diet, sleep and social situation may contribute to the bladder or the nervous system becoming more sensitive
- Emotional factors: many people can relate to the feeling of needing to do a ‘nervous’ wee, perhaps before an exam or a stressful situation. Screening questionnaires identify stress, anxiety, fear and panic
- Medical assessment: a GP or Urologist can investigate other factors that might be contributing eg hormones, prostate, neurological conditions
Physiotherapy Management of OAB
- Pelvic Floor Muscle Training – an individualised program that addresses the weakness or tension in the pelvic floor muscles and is progressed over time.
- Bladder/behavioural training – an individualised bladder training program breaks the cycle by using a range of strategies designed to suppress urgency resulting in arriving at the toilet feeling calm and in control
- Fluid intake advice – including types of fluid, volume and timing of fluid
- Lifestyle advice – general exercise, diet & sleep
- Mindfulness – understanding the physical and emotional response to bladder sensations and acting mindfully in response to urgency
- Stress management strategies –relaxation and breathing techniques
- Weight loss – reducing the pressure above the bladder with weight loss
- Transcutaneous Tibial Nerve Stimulation (TTNS) - Research has shown that stimulating the tibial nerve (located in the lower leg) can reduce the symptoms of OAB and increase bladder capacity. A small, portable TENS machine is used to stimulate the nerve for short periods every day at home
- Medication – there are a number of different medications for OAB prescribed by a doctor, often prescribed in combination with the strategies listed above.
- Medical referral – if symptoms are not improving an opinion from a GP and/or Urologist may be required
Don’t put up with OAB!
OAB is common, but not normal and can be successfully treated with the right assessment and an individual approach. If OAB if affecting day to day life for you or someone you know, it is time to take action and seek help.
March 2024