
Do you have pain in your bladder, rush to the toilet or go too often?
Bladder Pain Syndrome (BPS) is defined as persistent pain for greater than 6 weeks, in the bladder, urethra or perineal area (the area between your pubic bone and tailbone) that isn’t caused by an infection. People with BPS will often have a strong and regular urge to urinate.
BPS is similar to Interstitial Cystitis (IC) as the symptoms are alike. However, IC is diagnosed via an investigation called a cystoscopy, where a camera inside the bladder finds abnormalities in the lining of the bladder called Hunner lesions. BPS and IC are different to Overactive Bladder (OAB), where people will have an overwhelmingly strong urge to empty their bladder (without pain), and can sometimes leak on the way to the toilet. As you can see by the diagram, there can be an overlap of these symptoms, with both conditions experiencing frequent urination, both during the day and overnight.
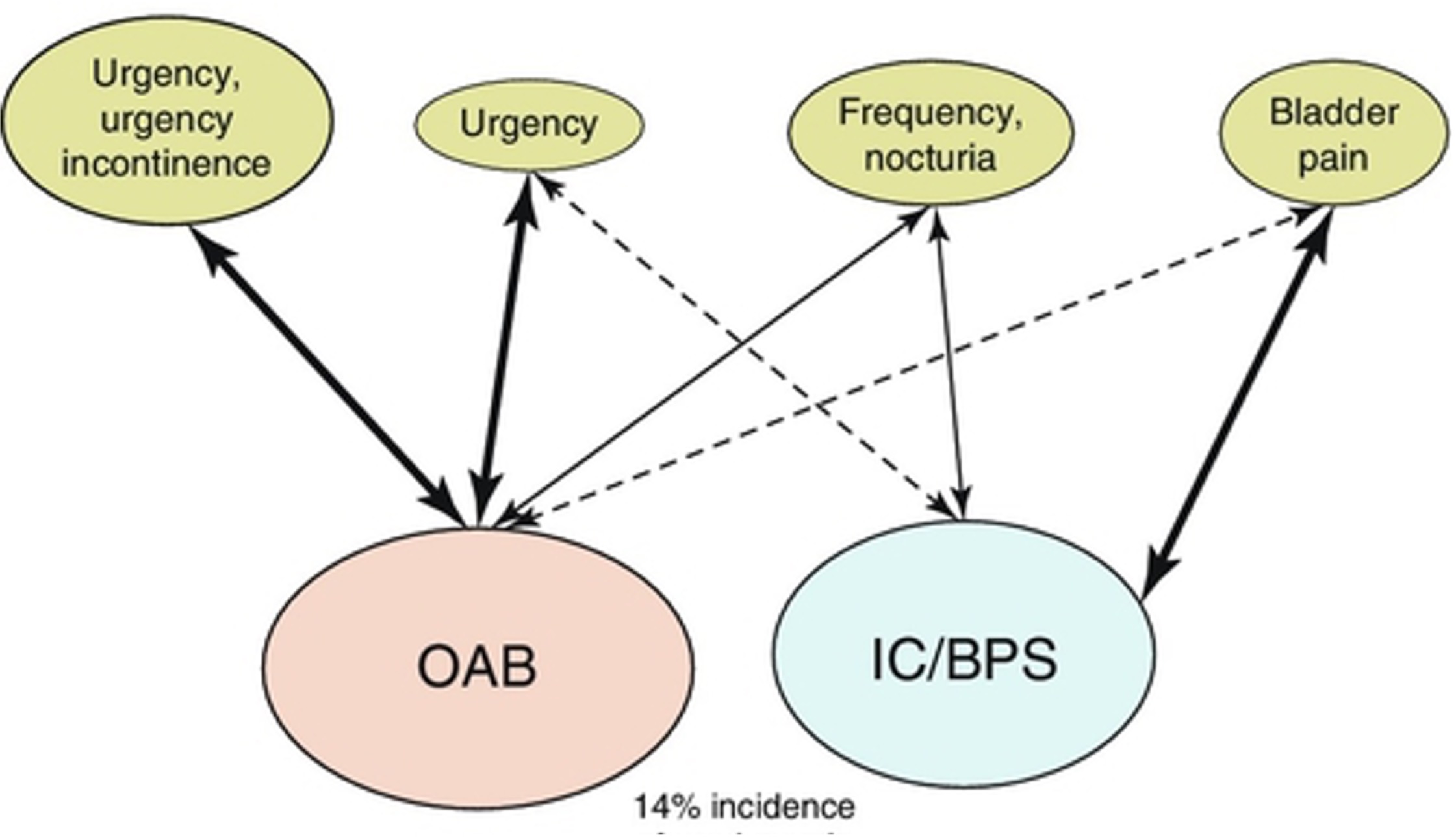
Milson et al, Abhams 2017
If you have bladder urgency and/or pain, it is important that you have a thorough assessment to determine your exact diagnosis, as there are other conditions that can cause bladder pain that need to be ruled out.
BPS is more common in women, accounting for 90% of cases. It is usually diagnosed in people in their 40’s but can occur at any age. People with BPS often have other co-existing health issues including fibromyalgia, irritable bowel syndrome, migraine, temporomandibular joint issues, endometriosis, chronic prostatitis, vulvodynia, depression and anxiety disorders. One thing we believe unites these co-existing conditions is a sensitised nervous system, which we will discuss later.
What are the symptoms of BPS?
Some people with bladder pain will experience regular symptoms, whilst others will only experience symptoms during ‘flares’.
Common symptoms may include:
- Lower abdominal, pelvic or urethral/bladder pain
- Pain or pressure as your bladder fills and/or when you wee
- Going to the toilet more frequently because of pain
- Having a constant feeling like you need to urinate, even after you have just emptied your bladder
- Feeling like you can’t hold much urine in your bladder
- Vaginal or vulval pain
- Pain in the scrotum, testes or penis
- Pain during and/or after sex
- Irritable bowels and/or constipation
It is very common for symptoms to be made worse by both physical and emotional stress. BPS can affect your social life, mental health, work, exercise, sleep and your relationships.
What causes BPS?
We are not sure of the exact cause of BPS and it could be due to a variety of factors. For some, symptoms may start after a bladder infection, repeatedly ‘holding on’ too long or after an autoimmune disorder flare up. For others, they may have another pelvic pain condition (eg Endometriosis or Irritable Bowel Syndrome) which leads to the bladder becoming sensitive.
There may be damage to the lining of the bladder wall allowing urine to leak into the bladder tissue which can irritate the nerves of the bladder which may result in pain and inflammation. It is also common that doctors cannot find any bladder tissue damage with investigations.
When pain is ongoing, there can be changes in the “motor” (movement) and “sensory” (feeling) areas of your brain that relate to your bladder or other pelvic organs. Your bladder and surrounding nerves can become more sensitive and your brain pays more attention to the messages coming from the bladder. As emptying your bladder is a vital body function, your brain is very protective of the bladder and pelvis and this can lead to pain and muscle spasm in the pelvic floor muscles and lower abdominal area.
One way to understand how your nerves become sensitised is to think about your nervous system like a car alarm that is programmed to be extra sensitive. Sometimes a car alarm goes off when just a leaf falls onto the windscreen. For someone with BPS, a small amount of urine in the bladder can set off the alarm, causing pain, urgency and muscle tension.
Treatment of BPS
Managing BPS can be challenging but it is very treatable. To support your recovery from bladder pain we recommend that you have a multidisciplinary team assisting you, involving a Urologist, GP and Pelvic Floor Physiotherapist, and sometimes a Pain Physician and Psychologist.
Pelvic Health Physiotherapy is recommended in international guidelines as one of the most appropriate initial treatments for the management of BPS.
How can Pelvic Health Physiotherapy help me?
Your Pelvic Health Physiotherapist will take a wholistic approach, assessing the physical, psychological and social factors contributing to your symptoms.
Treatment is based on your goals and is individualised to you. Treatment may include:
- Education: understanding how your brain, entire nervous system and body works together is important in reducing your symptoms
- Pelvic floor muscle relaxation exercises
- Breathing exercises to decrease stress and muscle tension
- Exercises to calm the nervous system and reduce the protective muscle spasm
- Bladder retraining and desensitisation
- Fluid intake and dietary advice
- Electrical stimulation to decrease pain and bladder sensitivity
- Stretching and strengthening exercises to decrease pain and improve movement
- Bowel management strategies
- Wellbeing and self-compassion strategies such as general exercise advice, sleep and stress management and mindfulness
Your Pelvic Health Physiotherapist will work with you to help you achieve your goals, restore pelvic health and empower you to live your best life.
February 2022




