Vulvodynia: Taking Understanding To a New Level
Vulvodynia is a chronic vulvar pain condition affecting 8-16% of women at some point in their lives1. It is the most common cause of sexual pain in pre-menopausal women.1 Despite the high prevalence and significant impact on quality of life, it remains poorly understood and often mis-diagnosed and mis-managed. With advances in pain neuroscience and central pain mechanism research over recent years, our understanding of vulvodynia has moved from a focus on local nociception to viewing it as a complex pain presentation. This demands a neurobiological and biopsychosocial approach to assessment and management1.
Recent high-quality evidence supports pelvic health physiotherapy as an effective first-line treatment for vulvodynia. A 2021 randomised controlled trial comparing multimodal physiotherapy2 to topical lidocaine found physiotherapy significantly more effective for:
- Reducing pain intensity during intercourse
- Improving sexual function
- Decreasing sexual distress
- Enhancing patient satisfaction
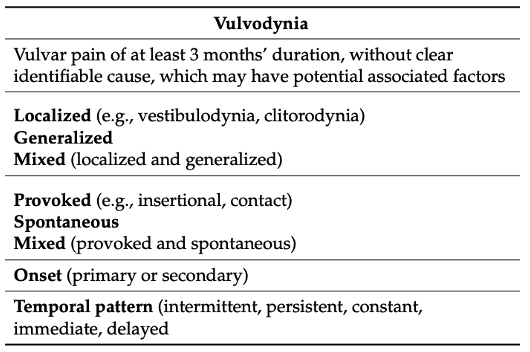
Definition and Classification
According to consensus terminology published in 20153, vulvodynia is defined as vulvar pain lasting at least 3 months without clear identifiable cause.
Provoked Vulvodynia (PVD) is the most common subtype, characterised by sharp, burning pain at the vaginal entrance in response to touch or pressure. This significantly impacts sexual function, relationships, and psychological wellbeing.
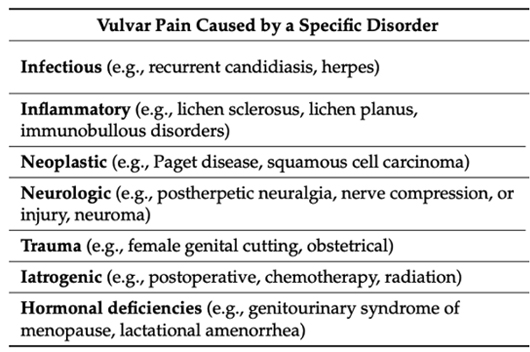
Other vulvar pain conditions that have an identifiable cause would not be classified as vulvodynia. These specific disorders are outlined in the table here.
Pathophysiology – A Neurobiological Perspective
When specific disorders causing vulvar pain have been ruled out, current evidence suggests vulvodynia is best understood as a complex pain condition involving a range of biopsychosocial predisposing and precipitating factors that lead to neurobiological changes1.
Biological Factors:
- Central pain processing changes and sensitisation including evidence of hyperalgesia and allodynia
- extending beyond the vulvar region
- Altered pelvic floor muscle tone, sensitivity and function
- Peripheral factors such as increased nerve fibre density in vestibular tissue
- Genetic predisposition
- Persistent inflammatory and / or infectious changes stemming from a history of recurrentbacterial or candida infections or tissue trauma
- Hormonal changes due to menopause, childbirth, medications
Psychological Factors:4
- Anxiety and depression
- Fear-avoidance behaviours
- Pain catastrophising
- Body image concerns
- Sexual anxiety and distress
- Post-traumatic stress in some cases
Social and Relational Factors:
- Impact on intimate relationships
- Partner responses affecting pain experience
- Communication difficulties
- Sexual script disruption (the set of ideas, behaviours, and expectations that guide how people think about and act in sexual situations)
- Cultural factors around sexuality
A Complex Pain Condition
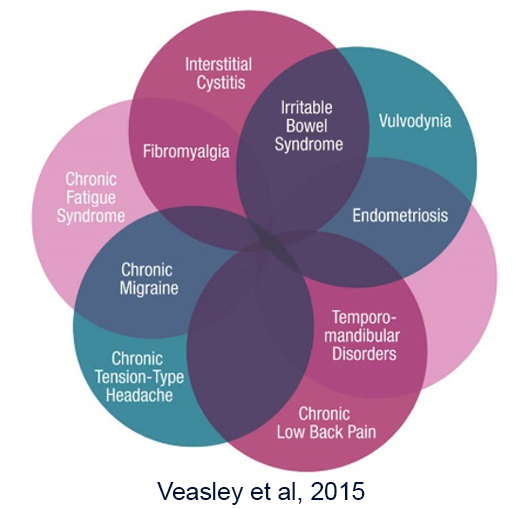
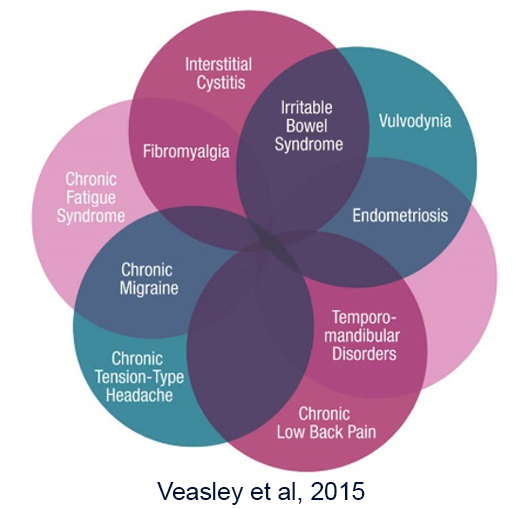
Vulvodynia is now considered to be one of the “central sensitisation syndromes”; a group of heterogeneous conditions characterised by persistent pain in the absence of clinically obvious pathology. Bladder Pain Syndrome, Irritable Bowel Syndrome, Chronic Fatigue Syndrome, TMJ and Fibromyalgia are all common comorbidities we see in clinical practice1.
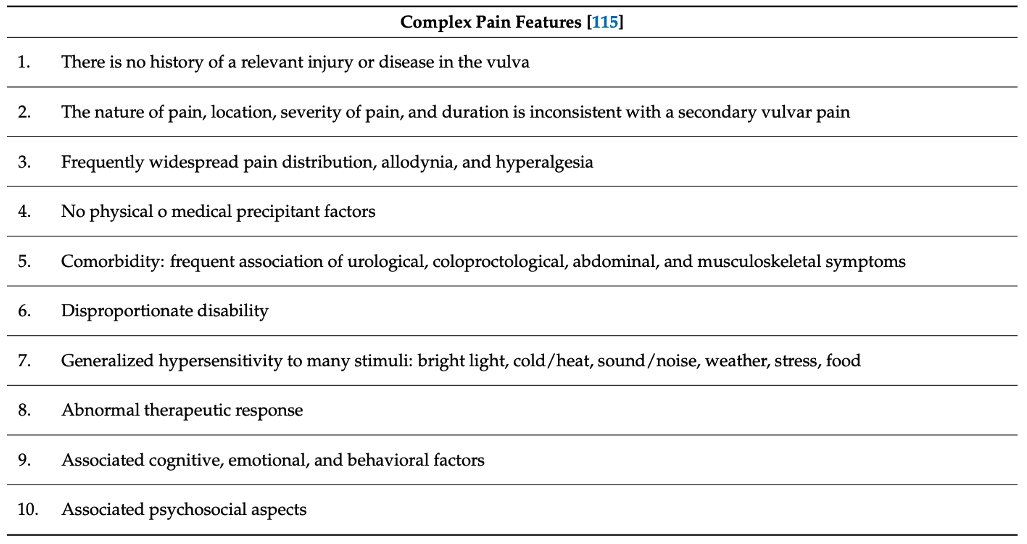
In 2021, Torres-Cueco1 et al outlined a complex pain identification system that aids in the recognition of persistent pain that is not associated with nociceptive input. It includes pain characteristics but also the commonly associated psychosocial and behavioural aspects of vulvodynia.1. Applying this clinical reasoning system can help to ensure we don’t fall into the trap of reducing vulvodynia to a mechanism or biomarker.
Pelvic Health Physiotherapy Assessment includes:
1. Detailed History and symptoms, medical, surgical and gynaecological history
- Pain characteristics, patterns & symptoms (using the Complex Pain Features table above)
- pain is often described as a burning, irritation sensation around the vulva and vestibule
- other symptoms include stinging, throbbing, and itching at the vaginal opening
- pain with sexual activity, tampon use, wearing tight clothing and sitting for long periods
- Previous investigations
- Previous treatments and effect of these
- Impact on function and quality of life
- Co-morbid conditions
2. Consider Central Mechanisms
- The Central Sensitisation Inventory is a simple and valid assessment tool that screens for the presence of central pain mechanisms/central sensitisation.6
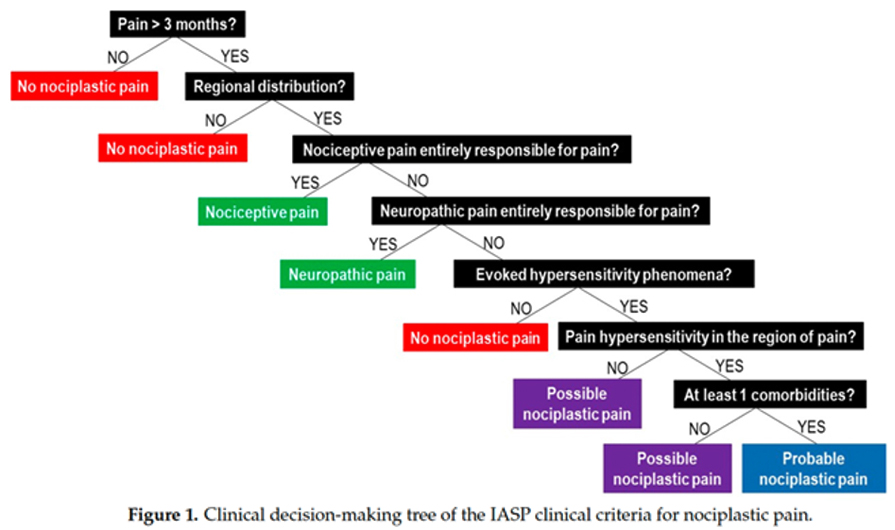
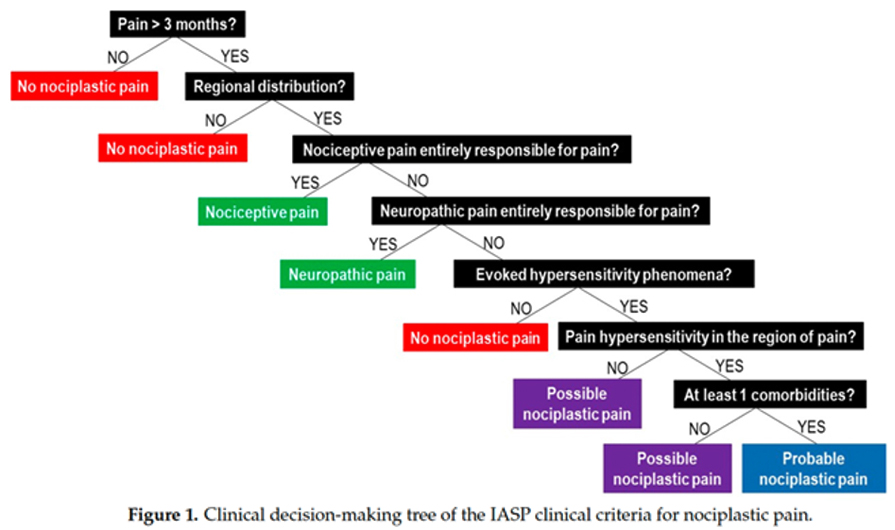
- Clinical decision making utilising the IASP clinical criteria for nociplastic pain such as that described by Nijs et al in 2023 (shown here as a decision-making tree) can assist clinicians to identify the presence of central drivers,7
3. Psychological Screening
Screening for psychological distress should be a routine component of all health professional’s assessment of vulvodynia. Understanding the cause and impact of emotional health on symptoms can provide invaluable clues to guide and prioritise treatment.
We advocate for a minimum of screening for4:
- Anxiety and depression; as both can precede and exacerbate vulvar pain, may be central pain drivers and are associated with reduced sexual function and satisfaction
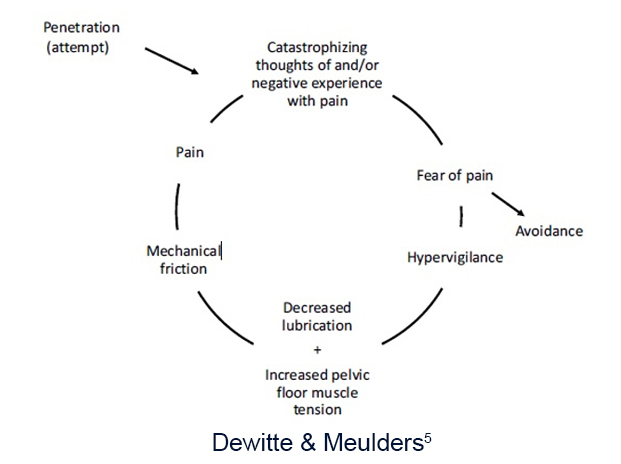
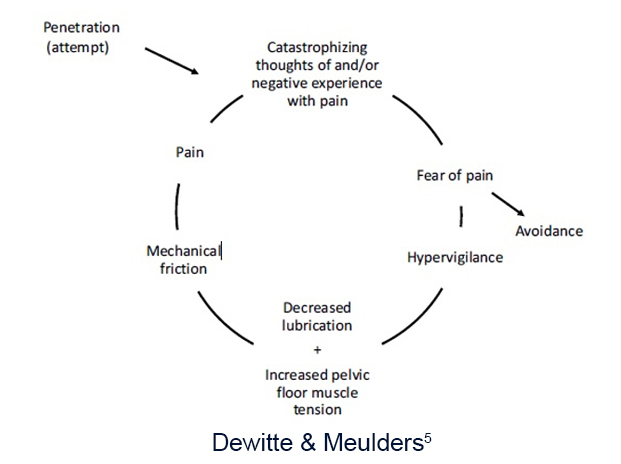
- Pain catastrophising; where fear of pain during intercourse, catastrophic thoughts about pain and hypervigilance to pain sensations can contribute to the vicious cycle of pain
- Fear-avoidance behaviours ie avoiding sexual activity and intimacy, withdrawal from relationships, increasing social isolation
- Screen for trauma and adverse childhood experiences
- Endurance Pattern; where people will continue with painful intercourse despite pain.
4. Sexual function assessment
- Sexual function questionnaires eg Vulvar Pain Functional Questionnaire, Female Sexual Function Index
- Questioning regarding sexual desire and arousal, sexual confidence and impact on sexual identity
5. Relationship impact; Communication difficulties with partners
- Fear of relationship breakdown
- Sexual anxiety and avoidance
- Partner responses affecting pain experience
6. Body Image and Self-Esteem
- Negative genital self-image
- Reduced body-exposure confidence
- Feelings of sexual inadequacy
- Impact on feminine identity
7. Physical Examination: A
trauma informed approach is essential and physical assessment should proceed at a pace determined by the patient following fully informed consent prior to and during the examination.
- Rule out other conditions according to vulvodynia diagnostic criteria
- Map pain location – a cotton swab test assesses vestibular sensitivity8
- Assess pelvic floor muscle function; pain, tension, contraction and relaxation, co-ordination and flexibility
Multi-modal, Multi-disciplinary individualised treatment approach
Evidence supports multimodal treatment that is evidence based, addresses the individuals main contributing physical and psychosocial factors, involves shared-decision making, is trauma-informed and collaborative.
In our opinion, a universal approach to management should include the following, irrespective of which health practitioner does the initial evaluation and education.
- Validation and hope are the most important aspects of initial care as people with vulvodynia have been frequently told the symptoms are “in their head” and they should simply relax or have a glass of wine for sex to be comfortable. It is vital to hear the story, understand beliefs and help make sense of the symptoms.
- Patient-Centered Care at all times that respects patient preferences, cultural sensitivity, is matched to their readiness and focuses on facilitation and not fixing to building self-efficacy and therapeutic alliance.
- Early Intervention that includes prompt referral to appropriate practitioners and services to prevent psychological deterioration.
- Integrated Care where there is co-ordination between healthcare providers, consideration of timing of referrals, written communication, a whole person approach and recognition of psychological needs.
- Treatment Planning should include value-driven goal setting and consider patient preferences and readiness for different interventions, partner involvement, and timing and pacing of interventions
- Educational Components don’t belong to any particular health discipline and are most effective when repeated, reinforced, consistent and the patient receives the information from a range of trusted health care practitioners. This education should include pain neuroscience education, psycho-education, sexual health information, appropriate lifestyle modifications, self-management strategies and where appropriate, partner education.
- Supported Self-Management such as the development of coping strategies, pain management techniques, communication skills and sexual confidence building.
- Monitoring Progress with regular re-assessment, tracking of relevant outcome measures, adjustment of approaches and recognition of psychological improvements.
Medical Management may include topical medications such as compounded amitriptyline, pain medication when appropriate and treatment of comorbid conditions.
Psychological management includes a range of approaches such as Cognitive Behavioral therapy, Acceptance and Commitment Therapy, mindfulness-based approaches, pain coping strategies, addressing fear-avoidance, sexual therapy and partner involvement where appropriate.
Pelvic Health Physiotherapy; Evidence & Approach
The Morin et al2 multimodal approach included pain neuroscience education, vulvar anatomy and function, healthy vulvar care practices, sexual health promotion and chronic pain management strategies. It also included pelvic floor muscle relaxation techniques, breathing exercises, general exercise promotion, desensitisation, graded exposure to feared activities, development of coping strategies, partner education and involvement and addressing fear-avoidance behaviours.
The outcomes of reduced sexual pain intensity, improved sexual function, decreased sexual distress and enhanced patient satisfaction were maintained at 6-month follow-up, with 79% of physiotherapy participants reporting being "much" or "very much" improved compared to 39% in the lidocaine group.2
An emerging physiotherapy approach called Somato-Cognitive Therapy9 emphasises patient empowerment and self-management while addressing both physical and psychological aspects of vulvodynia. This approach which aligns closely with the one we take at WMHP combines:
- Development of therapeutic alliance; building trust and rapport, collaborative goal setting and patient empowerment.
- Bodily exploration and awareness training; Movement exploration, breathing awareness, recognition of muscle tension recognition and the development of mind-body connection, understanding their genital anatomy and pleasure.
- Education; understanding pain mechanisms, the role of psychological factors and impact on sexual function, sexual desire, libido, arousal and use of lubrication.
- Cognitive restructuring; Identifying negative thought patterns, challenging unhelpful beliefs, developing adaptive coping and addressing fear-avoidance by creating safety through movement and touch.
- Structured homework; that includes graded exposure exercises, remapping any sensori-motor dysregulation, relaxation techniques, partner activities and self-exploration tasks.
Future Directions
Further research is needed regarding optimal treatment protocols and dosage, predictors of treatment response, timing of involvement of various disciplines, cost-effectiveness of different approaches, long-term outcomes and implementation strategies to improve access to care.
Success in treating vulvodynia relies on addressing the complex interplay between physical symptoms and psychological impacts. Healthcare providers should ensure everyone experiencing this condition has access to a comprehensive biopsychosocial management approach, tailored to individual needs and circumstances. Focus should remain on improving function and quality of life such as pleasurable sex rather than simply reducing pain.
References
1. Torres-Cueco R, Nohales-Alfonso F. Vulvodynia-It Is Time to Accept a New Understanding from a Neurobiological Perspective. Int J Environ Res Public Health. 2021 Jun 21;18(12):6639. doi: 10.3390/ijerph18126639. PMID: 34205495; PMCID: PMC8296499.
2. Morin, M., Dumoulin, C., Bergeron, S., Mayrand, M. H., Khalifé, S., Waddell, G., ... & Brochu, I. (2021). Multimodal physical therapy versus topical lidocaine for provoked vestibulodynia: a multicenter, randomized trial. American journal of obstetrics and gynecology, 224(2), 189-e1.
3. Bornstein, J.; Goldstein, A.T.; Stockdale, C.K.; Bergeron, S.; Pukall, C.; Zolnoun, D.; Coady, D.; consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal Disease (ISSVD); the International Society for the Study of Women’s Sexual Health (ISSWSH); the International Pelvic Pain Society (IPPS). 2015 ISSVD, ISSWSH and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet. Gynecol. 2016, 127, 745–751.
4. Chisari, C., Monajemi, M. B., Scott, W., Moss-Morris, R., & McCracken, L. M. (2021). Psychosocial factors associated with pain and sexual function in women with Vulvodynia: A systematic review. European journal of pain (London, England), 25(1), 39–50. https://doi.org/10.1002/ejp.1668
5. Dewitte, M., & Meulders, A. (2023). Fear learning in genital pain: Toward a biopsychosocial, ecologically valid research and treatment model. Journal of Sex Research. Advance online publication, https://doi.org/10.1080/00224499.2022.2164242
6. Neblett, R, Hartzell, MM, Cohen, H, Mayer, TG, Williams, M, Choi, YH. Ability of the Central Sensitization Inventory to Identify Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample. The Clinical Journal of Pain 2014; 31(4).
7. Nijs J, Lahousse A, Kapreli E, Bilika P, Saraço I, Malfliet A et al. Nociplastic Pain Criteria or Recognition of Central Sensitization? Pain Phenotyping in the Past, Present and Future. J. Clin. Med. 2021; 10, 3203. https://doi.org/10.3390/jcm10153203
8. Frawley H, Shelly B, Morin M, Bernard S, Bø K, Digesu GA et al. m An International continence society (ICS) report on the terminology for pelvic floor muscle assessment Neurourol Urodyn. 2021;1–44.
9. Kaarbø, M. B., Danielsen, K. G., Helgesen, A. L. O., Wojniusz, S., & Haugstad, G. K. (2023). A conceptual model for managing sexual pain with somatocognitive therapy in women with provoked vestibulodynia and implications for physiotherapy practice. Physiotherapy Theory and Practice, 39(12), 2539-2552.