Remapping Exercises For Sensorimotor Dysregulation: The What & The Why
The concept of sensorimotor retraining gained national and international attention in 2022 when a group of Australian researchers found promising benefits of graded sensorimotor retraining on pain intensity in patients with chronic low back pain. Known as the RESOLVE1 study, they used a framework that included graded, novel precise exercises which showed statistically significant improvements in pain. As movement therapists it is important that Physiotherapists understand how changes in sensorimotor representation within a sensitised nervous system requires us to move beyond typical therapeutic stretching and strengthening exercises. We take a deep dive into the neuroscience behind this and explain how remapping exercises can target the sensorimotor dysregulation contributors to persistent pelvic and sexual pain.
Brain Maps & Neurotags
Everything we do is programmed and recorded by the brain in unique patterns involving millions and millions of neurons. These patterns live in the Somatosensory Cortex of the brain and function just like a map. They include step by step instructions on how to do different activities efficiently and easily. These maps, evolving with practice, enable us to perform movements automatically.
Imagine if every time you button up your shirt you had to think about each step; how to hold the button, how to manipulate the buttonhole and how to slide the button through the buttonhole. Brain map allows us to do this complex task easily, without having to consciously think about it.
Each time we develop a map in our brain, a collection of neurons can also attach to it, in what we call a ‘neurotag’. The neurotag is like a graffiti tag, a ‘signature’ of brain activity. When our senses detect something, eg a sensation or a smell or a taste, thousands of neurons will ‘switch’ on at the same time. Neurons then learn to link each other, forming a ‘neurotag’ and as these groups of neurons grow, the neurotag becomes stronger.
Thinking back to the task of buttoning up a shirt, imagine if you had a cut on your thumb and it was painful to button up your shirt. You could choose to:
- Stop wearing shirts with buttons
- Change the way your button your shirt so that it doesn’t hurt*
- Keep buttoning your shirt the same way, despite it being painful**
*If you find a non-painful way to button your shirt, your brain will start to form a new map of this new movement. If you continue to button up your shirt this way for a period of time, this new map may actually become your new normal, even though it might not be the most efficient way of doing this task.
**If you keep buttoning your shirt in the same way and it continues to be painful, you may develop a new map for buttoning your shirt which now has a pain neurotag attached to it. This pain map can become your ‘new normal’, meaning it can continue to hurt when you button your shirt even after your thumb has healed. This is one way that persistent pain develops.
This concept of brain maps changing and becoming linked with pain is extremely common for people that experience pain. In fact, in people with persistent low back pain, 90% develop changes in the mapping areas of the brain2.
Altered Body Representation in Persistent Pain
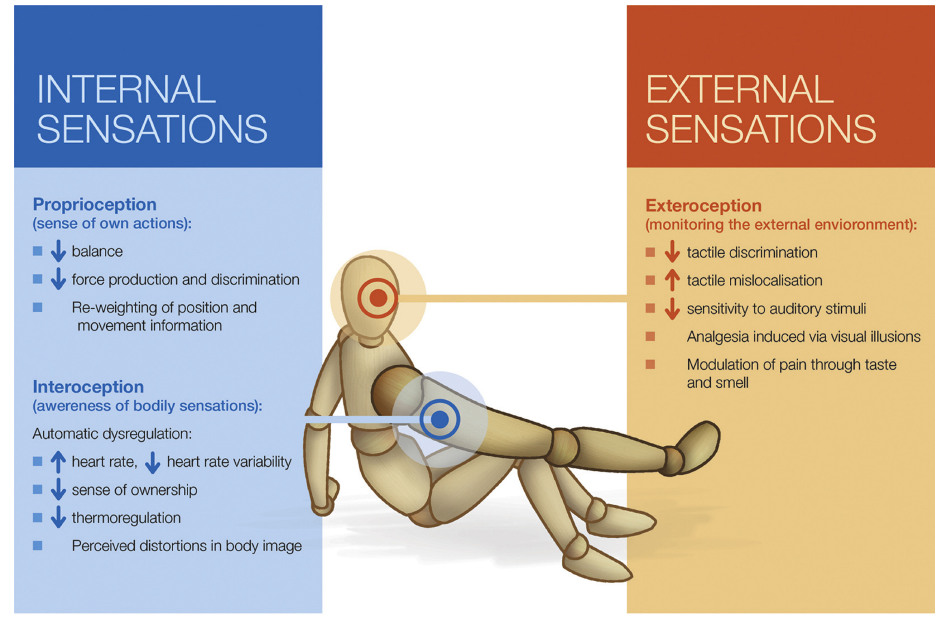
We now have growing evidence that persistent pain conditions have an associated central pathology involving cortical re-organisation, altered neural processing and an incongruence between expected and actual sensorimotor feedback. In a fascinating review of the subjective appraisal of body representation in people with persistent pain, Tsay3 et al examine the overlap of three broad sensory systems; proprioceptive information, exteroceptive stimuli and interoceptive awareness. They provide an overview of the literature that implicates distorted mental body representation in the presence of persistent pain as shown in this diagram and provide evidence for a multisensory and multimodal approach to therapies.
Pain Changes Movement & Sensory Awareness in The Pelvis
Pain prompts us to adapt our movements to avoid discomfort. In the pelvis, one or many painful or traumatic experiences with sex can lead to the pelvic floor muscles becoming tense and spasming involuntarily when insertion of a tampon, finger, penis or speculum is attempted in the future. For sufferers of Endometriosis when menstruation is painful, the pelvic and abdominal muscles often will tense and tighten as a natural protective response. For those with painful bladder or irritable bowel syndrome, sensory and motor signals are impacted and changed.
This in turn leads to alterations in the way the pelvis, perineum, pelvic floor, vagina, genitals and pelvic organs are mapped in the brain. The dysregulation of these sensorimotor maps can be addressed through detangling the motor programs and decreasing sensations that are being over-interpreted (hypersensitivity), under-represented (hyposensitivity) or mis-interpreted (dysesthesias).
We Can Measure If Brain Maps Have Changed
The Fremantle Awareness Questionnaire was developed by a group of researchers in Fremantle, WA and measures the degree of sensorimotor dysregulation that may be occurring with a particular body part. The questionnaire was originally designed to measure sensorimotor changes for low back pain and has been validated to do so. The questionnaire has now been expanded to measure knee, neck and shoulder pain and more recently, perineal pain.
At WMHP, we regularly screen our patients using the Fremantle Awareness Questionnaire and the Fremantle Perineal Awareness Questionnaire, which helps us to target our treatment selection more appropriately.
What Are Remapping Exercises?
Remapping exercises are novel, functional movements that aim to create new experiences for the brain and nervous system, generating a brand-new map of the symptomatic or painful area. The exercises are designed to change how people with persistent pain process sensations from their body and how they move. These practices involve soft, flowing movement, incorporating visual feedback and visual imagery. They can also include proprioceptive training to enhance awareness of body position and movement as well as graded motor imagery techniques to engage the brain in visualising and executing precise movements, without pain.
Stimulating different regions of the brain together makes the movements fresh and non-threatening for the nervous system allowing the brain to create new maps of the experience of moving the body. Some of these remapping practices are global, addressing the whole body such as Qi Gong4 whilst others are more specific to an area. With regular practise the default strategies or maps currently fused with pain, will weaken and the new maps, fused with relaxation and new visual images, will strengthen.
For remapping exercises to be effective, the correct type of exercise needs to be prescribed at the right time by a trained health care provider, with feedback given for performance. In the RESOLVE study, participants underwent 7 weeks of enhanced functional movement training, with mirror-visual and other forms of feedback. The training was conducted in a supervised session once per week, and also performed at home every day.
At Women’s & Men’s Health Physiotherapy, all of our physiotherapists have undergone further training in the science, theory and execution of remapping exercises for sensorimotor dysregulation. We have access to an extensive huge library of video resources that are individually prescribed and shared with our patients. In our clinical application of these exercises, we would firstly teach and demonstrate the exercises and observe the patient performing them so that we can provide feedback on their technique. We would then prescribe the exercise for them to perform at home, every day for a finite period of time, before reviewing them, reassessing the performance and effectiveness of the exercise and adapt or progress as required.
If you are interested in learning more about sensorimotor dysregulation and remapping exercises, Reframe Rehab run an incredible intensive course through Embodia.
References
1 Bagg M, Wand BM, Cashin AG, Lee H, Hubscher M, Stanton TR et al. Effect of Graded Sensorimotor Retraining on Pain Intensity in Patients With Chronic Low Back Pain. JAMA. 2022; 328(5):430-439. 10.1001/jama.2022.9930
2. Wand, B., Catley, M., Rabey, M., O’Sullivan, P., O'Connell, N., & Smith, A. Disrupted Self-Perception in People With Chronic Low Back Pain. Further Evaluation of the Fremantle Back Awareness Questionnaire. The Journal Of Pain. 2016; 17(9): 1001-1012. Doi: 10.1016/j.jpain.2016.06.003
3. Tsay, A., Allen T.J., Proske, U., Giummarra M.J. Sensing the body in chronic pain; A review of psychophysical studiers implicating altered body representation. Neuroscience and Biobehavioural Reviews 2015; 52, 221-232
4. Wang C, Schmid C, Rones R, Kalish R, Yinh J, Goldenberg D et al. A Randomized Trial of Tai Chi for Fibromyalgia. New England Journal of Medicine. 2010;363(8):743-754.