Explaining Pain Doesn’t Have To Be Painful
The research is now undeniable - educating a patient about the science of pain is an essential component of persistent pain care. Unfortunately, pain education is not easy and finding the right language is challenging for many health professionals.
We know that education is therapy but just like all education, there is no one size that fits all. Everybody has a different story, different ways of learning, a different lived pain experience, different culture, different pelvic pain presentation and different biopsychosocial contributing factors. The skill and the ‘art’ of pain education lies in being able to nuance the core messages (the target concepts we explore below) in a way that makes sense to and for the patient.
All target concepts in this article are directly extracted from Explain Pain Supercharged, Moseley & Butler, 2017 (a must read for anyone dealing with patients with chronic pain)
Target Concept # 1
Pain is normal, personal and always real
Many people with chronic pelvic pain have been told that their pain is ‘all in their head’. However, this is not true. Pain is NEVER imagined. If you feel pain, you have pain. Pain is a very individual and personal experience.
Target Concept #2
There are danger sensors, not pain sensors
There are no pain sensors, pain pathways or pain nerve endings. There are nociceptors, but nociception is just one of many inputs into the brain. Nociceptors can be thought of as ‘danger sensors’. The brain analyses all the different incoming messages and the brain decides whether you will feel pain, and the level of that pain.
Pelvic Pain is Different
Our brain responds to pain in the pelvis differently to pain in other areas of the body. The pelvis is responsible for 3 essentials of human life; reproduction, and elimination from the bladder and bowels, so when there is something wrong in the pelvis – the danger messages are amplified.
Target Concept #3
Pain and tissue damage are rarely related
Pain is an unreliable indicator of tissue damage. You can have pain, and no tissue damage. You can also have tissue damage, and no pain. This is a fact.
Prof Lorimer Moseley has a fantastic story explaining this concept, in a TED talk he presented in Adelaide.
Click here to watch this talk.
A helpful mantra to use with patients is “Hurt doesn’t equal harm”. This is especially relevant to pelvic pain patients who have had NAD investigations / laparoscopies.
Target Concept #4
Pain depends on the balance of danger and safety
Pain levels will vary, depending on the level of ‘DANGER’ or ‘SAFETY’ happening in a person’s life. In Explain Pain Supercharged, Moseley & Butler introduce the concept of DIMS and SIMS, and they aren’t talking about the steamed variety from the fish and chip shop!
What are DIMS and SIMS?
A DIM (Danger in Me) is anything that might be considered dangerous to your body tissues, life, job, happiness, or day to day function – anything which threatens who you are as a person , eg. stress at work.
A SIM (Safety in Me) is anything that makes you stronger, better, healthier, more confident, or happier within yourself or about yourself, eg. enjoying a walk along the beach with a friend.
Target Concept #5
Pain involves distributed brain activity
“There is no single pain centre in the brain. Pain is a conscious experience that necessarily involves many brain areas across time.”
When someone has been experiencing pain for an extended period of time, ‘neurotags’ are created, which are a pattern of brain activity – making it very easy for someone to feel pain. The brain can be described as an orchestra, in that it can find it difficult to learn a new tune, but once it has been playing the same tune for a long time (pain), it becomes very good at playing it.
Target Concept #6
Pain relies on context
Pain is influenced by everything happening in a person’s life. It can be influenced by your thoughts and beliefs, things you see, hear, smell and touch, the people in your life, things happening in your body and the places you go.
You will experience pain when your brain decides there is more likelihood of “danger” than “safety”, inferring the need to protect.
For example: You are walking across the road and you trip over and sprain your ankle. You probably would experience pain in this situation. However, if you were crossing the road whilst there was a big bus approaching you and you trip and sprain your ankle, you would probably quickly get back up and get to the other side of the road to get out of the way of the bus, feeling minimal pain. In both of these situations, the same injury could occur, but the pain experience may be very different
Target Concept #7
Pain is one of many protective outputs
When our body feels threatened, other protective systems (in addition to pain), can also be activated. These systems include the immune, endocrine, motor, autonomic / sympathetic, respiratory, cognitive, and emotional.
Have you ever had a patient with chronic pelvic pain, who also complains of fatigue, irritable bowels, anxiety, and potentially other diagnoses such as Fibromyalgia? Many of these associated symptoms can often be explained by a wound-up nervous system, with many of these systems becoming overprotective.
Target Concept #8
We are bioplastic
Our brains are constantly changing and adapting to everything happening in our lives. The longer you have pain, the brain adapts to be better and better at producing pain. However, all hope is not lost. Although the brains of people with chronic pain have changed, bioplastic changes in the brain will continue to happen until the day you die.
In the words of Prof Lorimer Moseley “Bioplasticity got you into this situation, and bioplasticity will get you out of it”.
Target Concept #9
Learning about pain can help the individual and the society
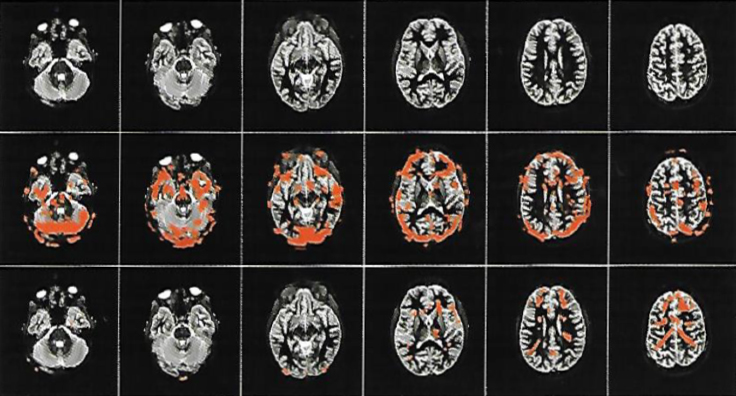
Who would have thought that learning about pain could be an effective therapy for chronic pain? This picture is proof that pain education works:
Image: Why Pelvic Pain Hurts: 2014 Louw, Hilton, Vandyken
- The first row in this picture is an MRI of someone who has had chronic pain for 3 years.
- The second row is the same person, and they have just completed a movement that gives them pain.
- The third row is the same person, doing the same activity, after learning about pain science for 30 minutes.
Target Concept #10
Active treatment strategies promote recovery
Have you experienced patients trapped in passive treatment strategies? Doctor shopping or looking for a ‘quick fix’ or a cure? Active treatment strategies, rather than passive, will promote recovery.
Once a patient understands their pain, they can make a plan on the road to recovery. Strategies such as improving physical fitness, eating better, sleeping better, increasing SIMS, and reducing DIMS all make a big difference to a person’s pain experience. With the help of our best friend bioplasticity, patients will see a slow and steady improvement over time.
Let’s Talk The Same Language About Pelvic Pain
When we are dealing with anyone in pain – language matters! We all owe it to our patients to have a better understanding of pain, and need to ensure we are speaking the same language.
Dr Marilla Druitt gives an excellent example of this in relation to endometriosis in an inspirational editorial in the O & G Magazine dedicated to Pelvic Pain (an absolute must read for anyone treating patients with pelvic pain): “Explain to women that we have no way of knowing what portion of their pelvic pain is due to endo, a muscle response, contributions from visceral hypersensitivity, other pain states or sleep and mood disorders – so EVERYTHING MATTERS – you can’t have pain if you don’t have a brain!!”.
Dr Druitt also finishes her editorial with a ‘call to arms’ which we 100% agree with: “If we are all better at treating pain, a little could go a long way. Gather your team – if not in a co-located fashion, in a virtual one – and endeavour to be on message as a group.”
If you want to learn more about Persistent Pain, here are some resources we recommend:
Explain Pain Supercharged. Moseley & Butler, 2017.
Therapeutic Neuroscience Education: Teaching Patients About Pain. Louw & Puentedura, 2013.
Why Pelvic Pain Hurts. Louw, Hilton & Vandyken, 2014.
Watson JA, Ryan CG, Cooper L, Ellington D, Whittle R, Lavender M et al. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J Pain 2019; Oct;20(10):1140.e1-1140
December 2019