Clitoral Curiosity
Every day, we speak with people who seek our support regarding painful sex. Often their stories include fear, confusion and a poor understanding of the vulva, clitoris and vagina. Many people hold unhelpful beliefs and perceptions of what is and isn’t normal.
Every member of the multi-disciplinary team supporting people experiencing dyspareunia plays a role in providing education. As part of the MDT, Pelvic Health Physiotherapists use education to empower individuals to develop a healthy perspective regarding their genitals and guide them toward safe, comfortable and pleasurable experiences with their body. Here we explore relatively recent discoveries regarding the clitoris and the relevance to those we see with pelvic health concerns.
We shared a version of this article on our patient blog, which was read by a record number of our readership, highlighting that many people are curious about the clitoris!
Pain Is A Passion Killer
This an important key message to share with patients. It is also important to explore what the term “sex” means to them. By definition, sexual behaviour refers to physical and psychological actions that involve sexual arousal, desire and satisfaction. Sexual activity is how we experience and express sexuality and includes a range of activities, from acts done alone to those with another person. Sexual activity is a fundamental aspect of human nature and is crucial in personal relationships, procreation, and individual well-being.
In validating our patient’s experiences, it is important we share messages that sex matters, it should never be painful, and in fact, it should be enjoyable and pleasurable. Unfortunately, 1 in 5 people assigned female at birth experience painful sex with many sufferers believing it is normal, it is their fault, that they weren’t aroused enough, or that there is nothing that can be done to help. We all know that this couldn’t be further from the truth!
It is normal to have a fluctuating level of desire and arousal, it is complex and influenced by many factors, including physical, psychological, circumstance, relationship, family & wider system and sexual contributors. Pain is one of those factors. Addressing desire and arousal, alongside other factors, is necessary for painfree and pleasurable sex.
Understanding Anatomy Helps
Society has perpetuated unhelpful myths about the names of our genitals, how they should look and what they do. This misinformation has led to confusion, worry and fear about what is normal. For many people, these negative thoughts and beliefs contribute to painful sex. Having an accurate understanding of the female genitalia creates a safe, healthy and realistic connection between the mind and the body. We should never assume how a patient views their genitals. The next time you are speaking to a patient experiencing dyspareunia, ask them some specific questions that explore their beliefs and thoughts about this area of their body.
Every Vulva Is Unique
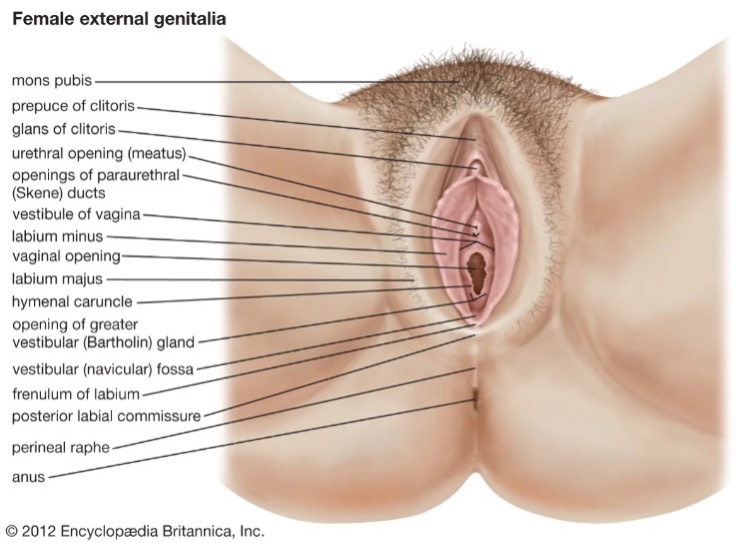 Most patients are surprised to learn that vulva’s are as different as faces! It can be enlightening for people to understand that whilst the parts that make up the vulva are the same, they can look very different from one person to the next. It is validating and helpful for people to realise that images appearing in magazines or pornography are often airbrushed or photoshopped (just like the one here!), giving a completely inaccurate representation of the variation that exists.
Most patients are surprised to learn that vulva’s are as different as faces! It can be enlightening for people to understand that whilst the parts that make up the vulva are the same, they can look very different from one person to the next. It is validating and helpful for people to realise that images appearing in magazines or pornography are often airbrushed or photoshopped (just like the one here!), giving a completely inaccurate representation of the variation that exists. To bust myths around female genitalia, Women’s Health Victoria has produced a wonderful online resource called The Labia Library, highlighting the variation and diversity in appearance that exists. Another wonderful resource, Flip Through My Flaps developed by Australian photographer, Ellie Sedgwick.
Get Curious About The Vulva & Clitoris
To overcome this fear, worry and pain, we encourage our patients to be curious about their vulva, to explore, with an open mind and without judgement what it looks like and what it feels like to touch. To explore with curiosity for curiosity’s sake can offer insight and confidence into what areas may feel comfortable and even pleasurable. For someone with pain, finding pleasure can take time. However, some attention on the only organ in the female body that exists purely for pleasure – the clitoris – can be a game changer.
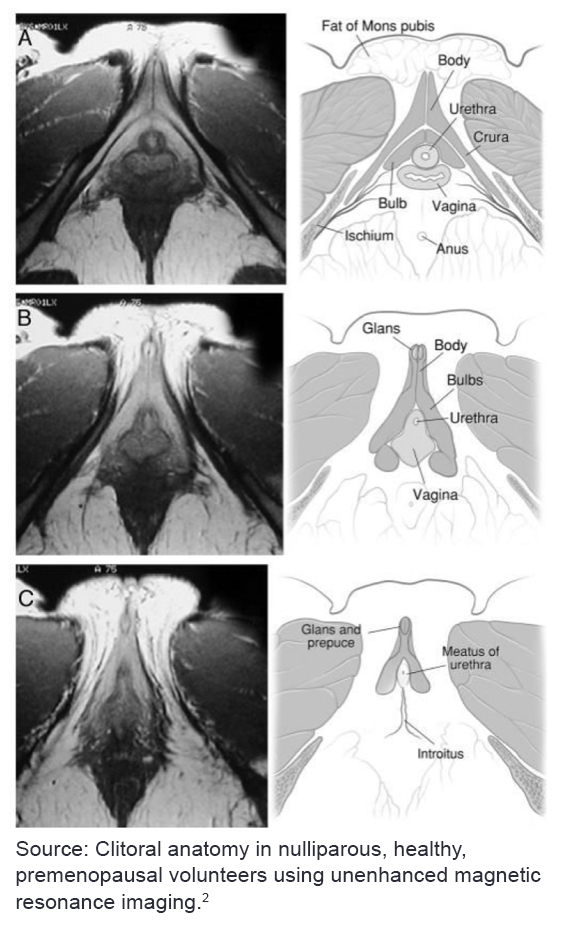 Perhaps unsurprisingly, many people cannot correctly identify the location of the clitoris on themselves or their partner. Until only recently, the anatomy of the clitoris was a mystery to the medical profession. It wasn’t until 2005, when pioneering Melbourne Urologist Professor Helen O’Connell published studies that mapped the extensive size, location and function of the clitoris.
Perhaps unsurprisingly, many people cannot correctly identify the location of the clitoris on themselves or their partner. Until only recently, the anatomy of the clitoris was a mystery to the medical profession. It wasn’t until 2005, when pioneering Melbourne Urologist Professor Helen O’Connell published studies that mapped the extensive size, location and function of the clitoris. Prof O’Connell showed through her research, that the clitoris is in fact, similar in size to that of a penis. It consists of a non-erectile tip (the glans), which is a small, button-like extension of the body of the clitoris, that sits external to the skin 1,2,3. Extending downwards from the glans is the remaining 90% of the clitoris, composed of two erectile bodies (the bulbs, crura and corpora)1,2,3. They have a relationship with both the distal urethra and vagina and are highly vascularised. When aroused, the
bulbs and crura become engorged with blood, placing pressure on the walls of the vagina, leading to more lubrication being produced. There are large neurovascular bundles that originate from the pudendal and cavernous nerves that supply the clitoris, and are actually visible to the naked eye on MRI imaging. 1,2,3
Professor O’Connell has candidly shared her story about what led to her eventually mapping the anatomy of the clitoris and the ongoing work she is doing to promote the importance of it in female sexual function. She, along with a group of other like-minded health professionals formed an alliance they named the ‘International Cliteratti’. To learn more, watch their recent ABC news interview.
Becoming “Cliterate”
Sex and pleasure should go together. When it doesn’t, we encourage anyone who owns a clitoris or cares about someone who does - to become curious about this incredible organ that exists purely for pleasure.
References
1. O’Connell HE, Sanjeevan KV and Hutson JM. Anatomy of the clitoris. J Urol. 2005; 174, 1189 –1195
2. O’Connell HE and DeLancey JOL. Clitoral anatomy in nulliparous, healthy, premenopausal volunteers using unenhanced magnetic resonance imaging. J Urol. 2005; 173(6): 2060–2063
3. O’Connell HE, Hutson JM, Anderson CR and Pelnter RJ. Anatomical relationship between urethra and clitoris. J Urol. 1998; 159,1892-1897
The following presentations were also sources of information:
Anita Elias. Sexual Medicine Specialist, Head of Sexual Medicine & Therapy Clinic, Monash Health. Deep Dive Into Dyspareunia Presentation; A Multidisciplinary Workshop on Sexual Pain. Monash University School of Medicine, Nursing & Health Sciences; 2024.
Anita Elias. Sexual Medicine Specialist, Head of Sexual Medicine & Therapy Clinic, Monash Health. Let’s Talk About Sex; Sexuality & Sexual Difficulties: An Introduction into Sexual Medicine & Therapy Presentations. Monash Obstetrics & Gynaecology; 2024
Christine Rafe, Sex & Relationship Therapist. Rebuilding Sexuality and Sexual Relationships with Pelvic Pain and/or Trauma. APA Webinar. 2023





