The Art & Science of Explaining Pelvic Pain
The evidence is now conclusive - educating patients about the science of pain is an essential component of treating persistent pain. Exploring how pain experiences are constructed in response to dangers and threats in our bodies and influenced by our thoughts, beliefs and context and the insight and knowledge gained throughout this process can be one of the keys to recovery. We first wrote a blog article on this topic in 2016; The Importance Of Pain Science Education that concluded with a call to action for clinicians working with persistent pelvic pain (PPP) patients - Considering biopsychosocial factors in PPP and combining these with pain science education provides an exciting new tool for effective management and hope for both patients and practitioners.
Effective pain science education (PSE) combined with physiotherapy has been shown to reduce pain intensity and disability in musculoskeletal pain, enhance participation in valued activities, increase adherence to active treatment approaches and most importantly improve pain self-efficacy. Until recently we haven’t had any research that looked at PSE in the pelvic pain population, here we explore recent developments in both the key PSE messages, the delivery and its application to PPP – it’s an art and a science. It is important to note that PSE, though vital, is not sufficient alone. It must be integrated with other treatment approaches to effectively address the complex, multidimensional nature of persistent pain, especially true when treating persistent pelvic pain.
The What & The How
In 2019 we wrote a follow up blog article titled “Explaining Pain Doesn’t Have To Be Painful” based on the 10 target concepts outlined in Explain Pain Supercharged, written in 2017 by Moseley & Butler1 and shared our experiences of applying these concepts to pelvic pain. These target concepts have since been further refined and reduced, often being informed by those with lived experience.
Lorimer Moseley, AO, incredible neuroscientist and pain science communicator has developed Essential Pain Facts2 in easy to understand language alongside visual images, adding to our tools for the What or content of pain science education. For clinicians who support people with pelvic pain and pelvic health conditions, these messages still need to be adapted appropriately to the pelvis.
PSE involves a two-way dialogue not a one-way didactic lecture and we now understand that How this education process occurs has a profound impact on its effectiveness. Clinicians have tended to take a “one and done” approach and simply delivered the pain science information which means they neglect to create a learning partnership with patients.3 Rather than a one-time event, effective PSE is woven throughout the therapeutic relationship, with concepts reinforced across multiple interactions.
While education itself is therapeutic, it must be a personalised process of sense making. Each patient brings their unique story, learning preferences, pain experience, cultural context, and biopsychosocial factors to both the therapeutic interaction and their ongoing reflective learning. The art of pain education lies in adapting core messages to resonate with the individual before us.
 Expert Consensus: A Framework for Pelvic Pain Education
Expert Consensus: A Framework for Pelvic Pain Education
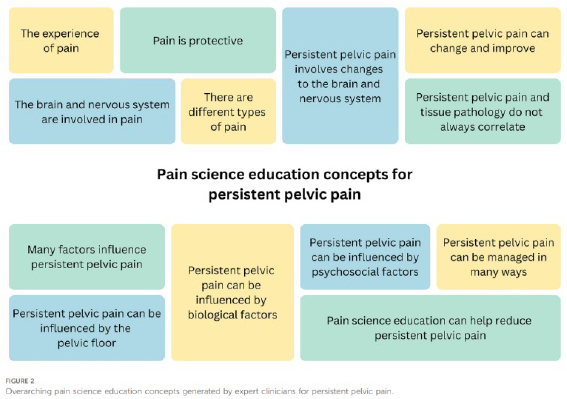
A 2025 expert consensus study by Mardon et al.4 established the first comprehensive framework for pain science education in persistent pelvic pain. Using e-Delphi methodology, researchers identified 125 learning concepts organised into 13 key categories. Shan Morrison, Director of Women’s & Men’s Health Physiotherapy was privileged to be involved in this study.
This framework provides clinicians with a roadmap and combined with further work by Mardon that we explore below, we now have evidence-informed education that acknowledges the unique aspects of persistent pelvic pain.
Patient Perspectives: What Concepts Matter Most
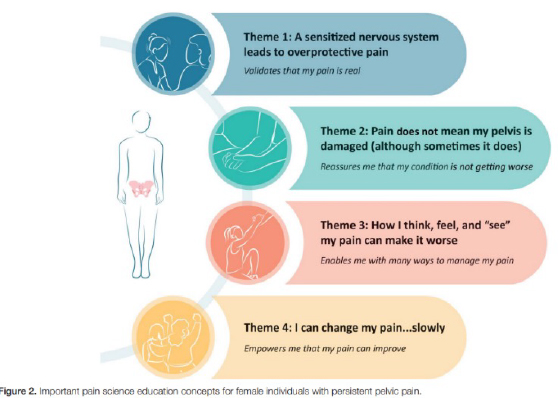 While experts provide the educational framework, understanding what resonates with patients is equally important. In fascinating and clinically applicable research titled I Wish I Knew Then What I Know Now, Mardon and colleagues5 performed a thematic analysis of qualitative data to identify PSE concepts that female individuals with persistent pelvic pain consider important and why. Four themes were generated that captured the PSE concepts considered most important by individuals who experienced improvements in their PPP.
While experts provide the educational framework, understanding what resonates with patients is equally important. In fascinating and clinically applicable research titled I Wish I Knew Then What I Know Now, Mardon and colleagues5 performed a thematic analysis of qualitative data to identify PSE concepts that female individuals with persistent pelvic pain consider important and why. Four themes were generated that captured the PSE concepts considered most important by individuals who experienced improvements in their PPP.Theme 1: A Sensitised Nervous System Leads to Overprotective Pain - validates my pain is real
Validation of pain is particularly important for individuals with pelvic pain because of the extensive history of prejudice and dismissal of their pain, particularly by healthcare professionals. Many patients describe feeling dismissed and being told their pain was "all in their head".
Understanding how persistent pain works and the changes in the nervous system helps patients recognise their pain as legitimate and provides a biological explanation for their experience. This validation can be especially meaningful for people who have previously blamed themselves for their pain.
Recognising this in our patients for many years, we shared a patient blog article titled Why Calming Down the Nervous System Can Help Endometriosis in 2021 that was also published on the Endometriosis Australia website.
Patient Stories:
"[The physiotherapist] showed me this picture of the brain with pain and the brain without and said 'okay actually there's these physical changes that have occurred in the brain'... It just made sense. All of a sudden, I'm like, 'Oh my god it's not me, it's not my personality, there's physical changes going on all this time'." (P152, endometriosis)
"Pain is pretty much always a protective mechanism, but your brain can't differentiate between what's like a real threat and what it thinks is a threat. So, it will essentially set up like this sensitisation process in which it's always going to keep thinking that like you're in danger, so it needs to protect you." (P6, vaginismus)
Theme 2: Pain Does Not Mean My Pelvis Is Damaged (Though Sometimes It Does) - reassures me that my condition is not getting worse
This concept helps patients understand the complex relationship between pain and tissue pathology, especially in endometriosis. Learning that increased pain doesn't necessarily indicate worsening of their condition provides reassurance and can reduce anxiety about movement and activity.
For those with conditions like endometriosis, acknowledging that pain can sometimes indicate pathology is also important, validating patients' experiences of receiving a diagnosis after years of suffering.
Patient Stories:
"I've learnt that pain doesn't equal damage, so that's been really important because when I thought pain equalled damage, I did everything I could to minimise pain, because I wanted to minimise damage. But I've learnt that that's not what's happening; that pain is the protect mechanism of the brain... I was scared of doing yoga —because I would hurt sometimes - and now I'm like, I'm back at yoga regularly." (P47, endometriosis)
Theme 3: How I Think, See and Feel can influence my Pain - enables me with many ways to manage my pain
Helping patients understand how psychological factors – thoughts and feelings - can influence their pain experience enables them to find multiple pathways to manage their pain beyond medication or surgery. Language used to describe pain, thoughts about pain, and the medical context all influence the pain experience. This is not to say pain is "all in their head," but rather that these factors provide additional avenues for modulating the experience of pain – in other words – everything matters.
Recognising this becoming an increasingly significant factor in our pelvic pain cohort during the global pandemic, we wrote an article in 2020 titled Stress, Anxiety & Pelvic Pain; a Challenging Combination and followed this up in 2023 with one titled Looking Outside The Pelvis In Persistent Pelvic Pain
Patient Stories:
"We looked at my trigger words which I think were, 'This is going to go on forever'. 'I have this the rest of my life'. 'This hurts so bad'. 'I'm in so much pain'. Then we had to look at shaping them to other things so that if I didn't exercise, or if I started feeling cramps, my brain didn't automatically go to those trigger words and then start that, 'Oh, there's pain. Let's make it worse'." (P19, endometriosis)
“I can see like the link with anxiety there, if like it’s making you anxious and you have pain, you’re less likely to do it because you think that there’s something physically wrong, which is just like a protective mechanism, but kind of a protective mechanism on steroids.” (P6, vaginismus)
“If you don’t understand how pain works, all the different suggestions seem, ‘How does that make sense… You’re asking me to exercise… moving hurts, exercise hurts. Why is this your suggestion?’” (P1, endometriosis)
Theme 4. I Can Change My Pain…….Slowly; empowers me that my pain can improve
Helping patients understand the concept of neuroplasticity—that the nervous system can change in response to experience—provides hope and empowerment. Understanding that pain is modifiable, albeit slowly, encourages patients to persevere with management strategies.
Patient Stories:
"I kept seeking other people to be the amazing healer in my life, and what I found through this 'Explain Pain' journey is that it has to be me. I have to be the one who is the magical healer of myself, and that's been quite a revelation." (P47, endometriosis)
A Final Word for Clinicians Supporting People With Persistent Pelvic Pain
Millie Mardon has provided us with invaluable information regarding what PSE target concepts are useful for those with PPP. The challenge remaining for clinicians is how to incorporate this into their management of PPP – which combines the science with the art form of patient-centered communication, weaving messages into patient conversations, providing lived experiences of change, relevant follow up resources and taking patients on a learning journey – over time.
Recognising that this cannot be achieved in one patient session, recent research by Núñez-Cortés6 on chronic spinal pain and further work by Mardon7 provide us with considerations for structuring effective pelvic pain education.
- Combine education with active treatment approaches ie movement, breathing, mindfulness and normalisation of pelvic floor muscle function.
- Provide approximately 200 minutes for pain intensity improvements and 150 minutes for disability improvements.
- Reflect on both content and delivery methods to achieve beneficial clinical effects.
- Tailor to individual patients, accounting for learning style, preferences and current beliefs.
References
1. Moseley GL, Butler DS. (2017). Explain Pain Supercharged. Adelaide: Noigroup Publications.
2. Pain Revolution; https://www.painrevolution.org/
3. Roose, E., Nijs, J., & Moseley, G. L. (2023). Striving for better outcomes of treating chronic pain: integrating behavioural change strategies before, during, and after modern pain science education. Brazilian journal of physical therapy, 27(6), 100578. https://doi.org/10.1016/j.bjpt.2023.100578
4. Mardon et al. (2025) Pain science education concepts for pelvic pain: an e-Delphi of expert clinicians. Front. Pain Res. 6:1498996.
5. Mardon AK, et al. (2024). "I wish I knew then what I know now" - pain science education concepts important for female persistent pelvic pain: a reflexive thematic analysis. PAIN, 165(6), 1-12.
6. Núñez-Cortés R, et al. (2024). The optimal dose of pain neuroscience education added to an exercise programme for patients with chronic spinal pain: a systematic review and dose–response meta-analysis. PAIN, 165(6), 1196-1206.
7. Mardon AK, et al. (2024). Recommendations for patient education in the management of persistent pelvic pain: a systematic review of clinical practice guidelines. PAIN, 165(6), 1207-1216.





