Bowel Function & Pelvic Health: The Underappreciated Link
Anorectal or bowel dysfunction is common, yet is under-reported, under-diagnosed and under-treated. Nearly 2% of Australian adults experience faecal incontinence and 4% experience both urinary and faecal incontinence1. A staggering 40% of the world’s population are impacted by Disorders of Gut-Brain Interaction (DGBI) eg Irritable Bowel Syndrome (IBS)2.
Other pelvic health conditions such as urinary incontinence, pelvic organ prolapse and pelvic pain often co-exist with bowel disorders. Therefore, any pelvic health condition should consider bowel function during assessment and management.
The Wide Spectrum of Anorectal Presentations
The spectrum of anorectal symptoms that pelvic health physiotherapists see is extensive. These can occur independently or co-exist:
- Faecal / flatal incontinence
- Involuntary loss of faeces (solid or liquid), flatus, passive faecal incontinence (soiling without sensation or warning or difficulty wiping clean)3
- Faecal urgency
- Sudden, compelling desire to defaecate that is difficult to defer3
- Feeling of incomplete evacuation
- Complaint that the rectum does not feel empty after defaecation3
- Straining to defaecate
- o The need to make an intensive effort (by abdominal straining or valsalva) to either initiate, maintain or improve defaecation3
- Constipation:
- Complaint that bowel movements are infrequent and/or incomplete and/or there is a need for frequent straining or manual assistance to defecate, based on Rome IV diagnostic criteria of4:
- Two or more of the following:
- Straining more than 25% of defaecations
- Lumpy or hard stools
- Sensation of incomplete evacuation more than 25% of the time
- Manual manoeuvres to assist with emptying more than 25% of the time
- Less than 3 spontaneous bowel movements per week
- Two or more of the following:
- Loose stools rarely present without laxatives
- Insufficient criteria for IBS
- Complaint that bowel movements are infrequent and/or incomplete and/or there is a need for frequent straining or manual assistance to defecate, based on Rome IV diagnostic criteria of4:
- Rectal Prolapse
- Protrusion of the rectum beyond the anus3
- Persistent Anorectal Pain4,5
- Levator Ani Syndrome
- Persistent or recurrent rectal pain, lasting more than 30 minutes, with tenderness with traction on puborectalis muscle
- Proctalgia Fugax
- Recurrent episodes of rectal pain unrelated to defaecation that lasts from seconds to minutes (maximum 30 mins), with no pain between episodes
- Levator Ani Syndrome
- Irritable Bowel Syndrome (IBS)4
- Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool
- There are different subtypes of IBS characterised by predominant bowel habits (constipation, diarrhoea, mixed or unclassified)
- Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
Anorectal Dysfunction Doesn’t Always Present As The Main Problem
In our clinical practice, anorectal dysfunction can be the primary complaint, a coexisting problem or a contributing factor.
It is well known that repetitive straining is a risk factor for Pelvic Organ Prolapse (POP)6 and urinary incontinence7. There is a strong relationship between overactive bladder and IBS, with some studies reporting a prevalence up to 33.3%6. Women with endometriosis are twice as likely to have an IBS diagnosis8.
Whatever the main concern, bowel function should always form part of the assessment process.
The Relationship Between Pelvic Floor Muscle (PFM) Dysfunction & Anorectal Conditions
There are multiple PFM dysfunction possibilities that may present as a component of the underlying pathophysiology of anorectal disorders. This is illustrated by the range of PFM assessment findings present in somebody experiencing constipation:
- Increased tone of the PFM which may result in poor relaxation during defaecation and contribute to incomplete emptying
- Weakness, poor support and increased descent of the PFM and connective tissue, impacting the mechanics of defaecation
- Poor coordination of the PFM, where the muscle contracts when it should be relaxing (defaecation dyssynergia) or vice versa
- In some cases, PFM function is completely normal and the constipation is due to other factors
Additionally, in people experiencing persistent pelvic pain and IBS, features of pelvic floor dysfunction or gynaecological and psychological factors can be related to their disordered anorectal function, but do not necessarily predict the outcome of a physical assessment5.
A thorough clinical examination by a trained Pelvic Health Physiotherapist is a vital component of the assessment process to determine if there is PFM dysfunction present, and if so, what the most appropriate PFM exercise program is for that individual.
The physical examination (with informed consent) may involve:
- A digital rectal examination (DRE) to determine resting muscle tone, ability of the EAS and levator ani to contract and relax (at the right time), endurance and coordination
- Observation of the perineum in a sitting position on a commode to understand structural support and defaecation dynamics
- Transperineal ultrasound to visualise the anorectal angle, levator plate, PFM contraction, relaxation and coordination during simulated defaecation
- Abdominal palpation to assess the tone, activity and co-ordination of the abdominal muscles during breathing and simulated defaecation
- Breathing pattern observation and assessment
Chicken Or The Egg: Psychosocial Implications
The impact of bowel symptoms on psychosocial distress can be substantial and significantly impact quality of life, regardless of symptom severity. We commonly hear stories from people who report:
- Fear of leaving the house if they haven’t emptied their bowel in the morning
- Avoiding eating or drinking food if they are planning on going out for fear of having an accident or an episode of urgency
- Needing to know where the closest toilet is at all times
- Feeling that their day is ruined if they haven’t emptied their bowel in the morning
The experience of fear, anxiety, hypervigilance and catastrophisation often leads to a sensitisation of their nervous system, which further reinforces the vicious cycle of their symptoms. Understanding the presence and impact of psychosocial distress is also an integral component of assessment and management of anorectal dysfunction.
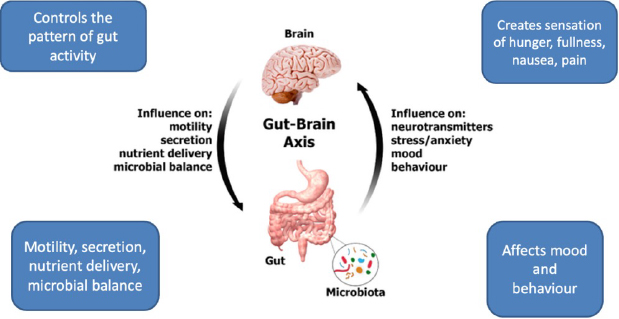
The Integral Relationship Between the Brain and the Gut
The gastrointestinal tract comprises the enteric nervous system, which has over 600 million neurons that convey information via the vagus nerve in a two-way communication pathway:
- from the brain to the gut carrying messages that control the pattern of gut activity
- from the gut to the brain creating sensations of hunger, fullness, nausea, pain, all of which can affect mood and behaviour
The vagus nerve plays an important role in connecting the autonomic, endocrine, immune and enteric nervous systems, as well as contributing to regulation of gut health with the emotional and cognitive areas of our brain. The vagus nerve, neurotransmitters and hormones all play a role in the complex relationship of digestion with sensations of fullness and hunger. 95% of the serotonin produced in the body is made in the gut, emphasising the strong link between emotional health and gut disorders.
Trauma and Anorectal Dysfunction
Evidence shows that people who have experienced physical, emotional and sexual abuse have higher rates of gastrointestinal symptoms than controls (including IBS)9. There are also numerous systematic reviews that establish a connection between a trauma history and IBS, inflammatory bowel disease (IBD), dyssynergic defaecation and constipation9. Sadly, it makes sense that a history of trauma can pre-dispose an individual to anorectal symptoms due to alterations in the hypothalamic– pituitary–adrenal (HPA) axis, which plays a central role in mediating the stress response and regulating the interaction between the gut microbiota, the gut and brain.
A trauma informed approach and understanding the sensitivity of a person’s nervous system is therefore a very important part of managing anorectal dysfunction. Jagielski et al9 describe several strategies that should be employed to support people that may require an anorectal examination:
- Prior to any assessment:
- Screen for trauma
- communicate and obtain initial informed consent
- Answer questions and validate concerns
- Cultivate a trauma informed environment
- During any assessment
- Obtain ongoing consent
- Monitor for signs of distress or dissociation
- After assessment
- Debrief with the patient
- Provide a written summary
- Refer for psychological support if needed
Anorectal Dysfunction Requires A Biopsychosocial Approach
Whilst anorectal dysfunction can be complex, with a biopsychosocial framework, sound clinical reasoning and a multidisciplinary team (eg GP, Gastroenterologist, Colorectal Surgeon, Psychologist, Gut Directed Hypnotherapist, Dietician and Pelvic Health Physiotherapist), it can be very successfully treated.
If anorectal dysfunction has been established as the primary complaint or a contributing factor to another pelvic health concern (ie OAB, POP), management of this dysfunction should be a priority10
From a physiotherapy perspective, once pelvic health goals have been established, we combine history and symptom information with psychosocial screening questionnaires, physical examination and a bowel diary to determine a management plan, which may include the following:
- Education
- Understanding normal bowel function can reduce fear and anxiety associated with symptoms
- Awareness of the gut-brain axis, the nervous system, pain system and musculoskeletal system and how they interact with emotional health and gut function
- Breathwork
- Diaphragmatic breathing can regulate the coordination of the diaphragm and PFM to descend and relax at the right time during defaecation
- Breathwork is an effective strategy to move out of a sympathetic state of flight or fight and into a parasympathetic state of rest and digest
- Defaecation dynamics
- Teaching correct defaecation dynamics is more than instructing someone to elevate their feet and bulge their belly when they sit on the toilet
- Technique must be assessed and the retraining individualised to ensure generation of enough rectal pressure without compromising pelvic floor support
- Establishing an effective bowel routine
- Many people don’t appreciate the importance of a routine that takes advantage of the HAPC – high amplitude propagating contractions of the smooth muscle of the bowel that occur upon waking and after meals
- PFM training (PFMT)
- The goal of PFMT may be to improve awareness, strength, relaxation, coordination or endurance
- PFMT will always be linked to functional requirements
- Application of adjunctive therapy ie Electrical Stimulation
- Biofeedback for PFMT can be provided via:
- Verbal instruction and feedback
- Palpation via DRE/abdomen
- Visual feedback via transperineal ultrasound
- Per rectal EMG biofeedback
- Rectal Balloon Therapy
- Rectal Balloon Assessment and Therapy
- To assess rectal sensation, compliance and defaection dynamics
- For sensory and/or defaecation retraining
- Abdominal massage has been shown to increase the frequency of defecation, improve defaecation dysfunction, stool consistency and quality of life11
- Urge Suppression Strategies
- To assist in calming the urgency sensation and break the fear-urge cycle
- Stool Manipulation
- Working in conjunction with a GP, dietician or medical specialist, we explore strategies to optimise stool consistency, within the scope of our clinical expertise
- Strategies to calm a sensitised nervous system
- Mindfulness, whole body movement practices, general exercise, sleep hygiene, stress management and more
Regardless Of Your Discipline, We All Should Care About Bowels
Given the prevalence and the under-reporting of anorectal dysfunction, it is imperative the assessment of bowel function and symptoms are a routine component of patient care. Whether the anorectal dysfunction is the primary or co-existing complaint, adopting a whole person, multidisciplinary, individualised approach will contribute to everyone living their best life.
References
1. Deloitte. 2024. Economic Cost of Incontinence in Australia. Continence Foundation of Australia
2. Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J et al. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. 2021 Jan;160(1):99-114.e3. doi: 10.1053/j.gastro.2020.04.014. Epub 2020 Apr 12. PMID: 32294476.
3. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee, J. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Floor Dysfunction. Neurourology and Urodynamics. 2010; 29:4–20
4. Rome Foundation. 2016. ROME IV Diagnostic Criteria for Disorders of Gut-Brain Interaction. (4th ed)
5. Engeler D, Baranowski AP, Berghmans B, Birch J, Borovicka J, Cottrell AM et al. EAU Guidelines on Chronic Pelvic Pain. European Association of Urology; 2024.
6. Finazzi Agrò E, Salvatore S, Braga A, DeLancey J, Fernando R, Iacovelli V et al. Pathophysiology of Urinary Incontinence, Pelvic Organ Prolapse and Faecal Incontinence. In: Cardozo L, Rovner E, Wagg A, Wein A and Abrams P eds. Incontinence. 7th Ed. 2023:247-396
7. Castro-Diaz D, Robinson D, Arlandis Guzman S, Bosch JLH, Costantini, E Cotterill N. Initial Assessment Of Urinary Incontinence. In: Cardozo L, Rovner E, Wagg A, Wein A and Abrams P eds. Incontinence. 7th Ed. 2023: 397-436
8. Yang F, Wu Y, Hockey R, Doust J, Mishra GD, Montgomery GW et al. (Evidence of shared genetic factors in the etiology of gastrointestinal disorders and endometriosis and clinical implications for disease management. Cell Reports Medicine. 2023; 4 (11): 101250
9. Jagielski, CH, Naftaly, JP & Riehl, ME. Providing Trauma Informed Care During Anorectal Evaluation. Curr Gastroenterol Rep. 2023; 25: 204 – 211 https://doi.org/10.1007/s11894-023-00879-4
10. Dumoulin C, Booth J, Cacciari L, Campbell P,Hagen S, Homsi J et al.Adult Conservative Management. In: Cardozo L, Rovner E, Wagg A, Wein A and Abrams P eds. Incontinence. 7th Ed. 2023: 795-1038
11. Gu X, Zhang L, Yuan H and Zhang M. Analysis of the efficacy of abdominal massage on functional constipation: A meta-analysis. Heliyon. 2023 Jul 7;9(7):e18098. doi: 1016/j.heliyon.2023.e18098. PMID: 37496907; PMCID: PMC10366436.z0
12. Wang J, Varma MG, Creasman JM, Subak LL, Brown JS, Thom DH et al. Pelvic floor disorders and quality of life in women with self-reported irritable bowel syndrome. Aliment Pharmcol Ther. 31; 424-431