Nocturia – More Than Just a Bladder Issue
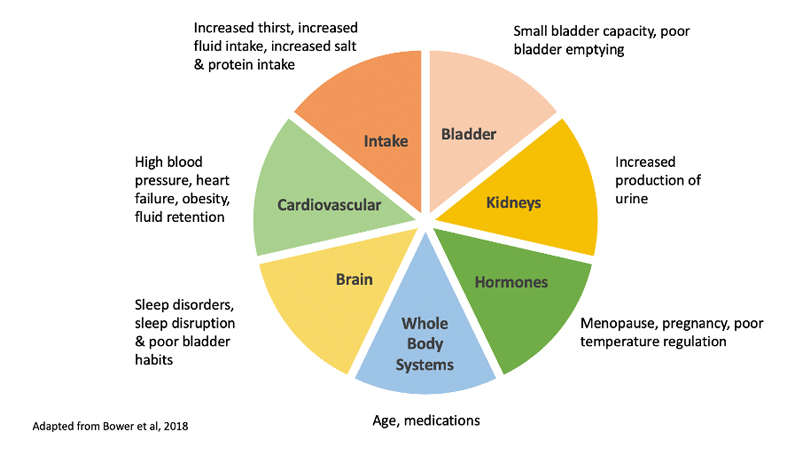
Multidimensional Nature
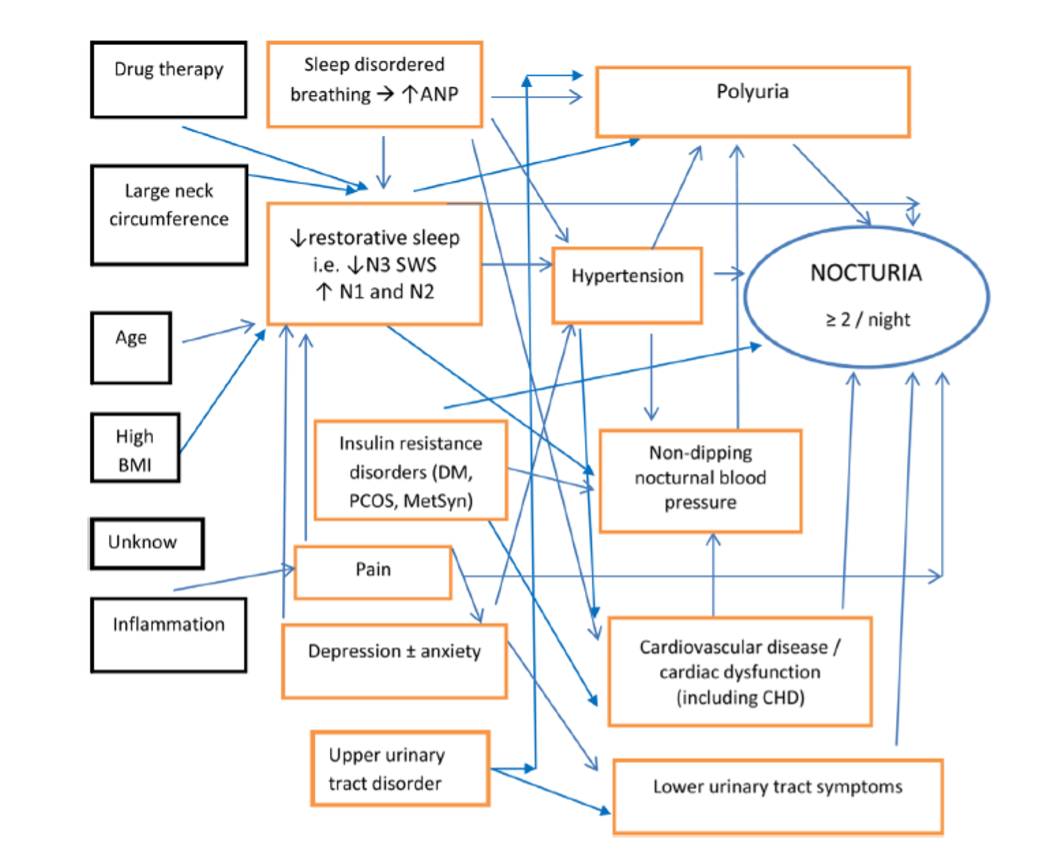
Summary of casual assumptions underlying nocturia with confounding variables in black boxes3
Recommended Nocturia Questions for GP’s:
- How many times do you wake up at night to pass urine?
Voids following being woken from sleep should be differentiated to ‘just in case’ voids when woken by sleep disturbance - How much does nocturia bother you?
Persistent nocturia impairs the quality of sleep, usually reducing the time per cycle in slow-wave sleep. A ‘First undisturbed sleep time (FUST)’of 3 hours or less is associated with high bother. - What medications are you taking?
Medications may induce diuresis or disturb sleep and should be specifically reviewed if a change has coincided with nocturia. - How much is your bladder actually storing day and night?
A bladder diary or frequency volume chart (FVC) over 48-72hrs is essential and patients should be thoroughly educated regarding the importance for diagnosis and management. Data on fluid intake, urgency, sensation of fullness, diurnal and nocturnal frequency and volumes combined with an ultrasound measure of post-void residual provides important information on bladder storage. - How much urine do you make overnight?
This will be identified by the FVC. Overnight urine output that exceeds 33% of 24-hour production indicates nocturnal polyuria, a common finding in up to 80% of those with nocturia - which will occur when nocturnal urine production exceeds bladder capacity. - Do you have hypertension or cardiac failure, with or without leg oedema?
When supine, blood pressure increases, increasing renal perfusion, potentially resulting in nocturnal polyuria. Antihypertensive medication swapped to being taken in the evening may reduce the volume of urine produced overnight. - Are you a good sleeper?
Obstructive sleep apnoea can result in increased blood pressure and nocturnal polyuria. Common symptoms are snoring loudly, episodes of suffocation during sleep and excessive sleepiness during the day. Other sleep disturbances may include insomnia, restless legs, anxiety, depression and environmental factors. - Have hormone levels be checked recently?
The net effect of all sex hormones is antidiuresis at night. Reduced oestrogen may result in nocturia, sleep disturbance and impaired wellbeing. Depletion of testosterone is associated with loss of muscle mass and bone strength, reduced bone density, sexual dysfunction, deterioration of insulin sensitivity, elevated visceral fat and metabolic syndrome – all of which may affect nocturia.
Assessment of Nocturia
- A general physical examination identifying any underlying disorders that may be impacting urine production and bladder storage or reducing arousal mechanisms. This should include:
- Urinalysis
- BMI +/- metabolic syndrome
- Lower limb oedema
- Cardiac disease, hyper or hypotension
- Neurogenic disease
- Blood tests to identify diabetes, heart, liver or kidney disease or sex hormone depletion
- TANGO screening tool – to identify clinically relevant co-morbidities (see below).
- Bladder diary – to assess lower urinary tract symptoms, total urine volume, nocturnal urine volume, nocturnal bladder capacity index.
- Sleep assessment – including when the patient goes to sleep, when they first wake, number of times they wake, and how long they sleep for.
TANGO – Targeting the Aetiology of Nocturia to Guide individualised treatment and improve Outcomes.
Dr Wendy Bower, physiotherapist and researcher at Royal Melbourne Hospital lead a research team in Australia, Europe and Asia that investigated nocturia, its multifactorial aetiology, and how to most effectively treat it. This team developed a screening tool identify clinically relevant co-morbidities, which in turn guides treatment direction. The TANGO tool has 23 questions over 4 domains:
- Cardio / metabolic
- Sleep
- Urinary tract
- Wellbeing
Intervention Strategies
- Optimising general health; management of hypertension, cardiac dysfunction and diabetes. Addressing appropriate physical exercise and lifestyle management.
- Bladder rehabilitation; treatment of OAB with bladder retraining, management of anxiety, fluid intake modification and medication.
- Reduction of nocturnal urine volume; reduction of lower leg oedema, fluid intake and dietary sodium and protein restriction, medication management e.g., timing of diuretic.
- Sleep prolongation; management of insomnia, sleep disorder, restless legs and night pain and addressing environmental influences.
Role of Pelvic Health Physiotherapy
- Bladder diary; fluid intake and urine output to thoroughly assess frequency, urgency, bladder capacity, sensation of fullness, and hydration habits.
- Bladder ultrasound: PVR- to check bladder emptying.
- UTI screening (dipstick): If not completed by a GP and refer on for MSU if relevant.
- Fluid and diet adjustments: Based on results of the bladder diary as part of bladder training.
- Bladder Training: to increase bladder capacity and manage strong urgency signals. Education re good bladder habits.
- Pelvic Floor Muscle Training: Strengthening or relaxing these muscles can improve bladder control and emptying.
- Constipation Management: healthy bowel habits positively impact bladder function.
- Sleep Hygiene: assessment of sleep, review of routines and sleep hygiene advice for getting to and staying asleep.
- Exercise Guidance: regular physical activity is linked to reduced nocturia and promotes general relaxation and better sleep.
Clinical Takeaways