Endometriosis, No More Suffering In Silence
Key Messages
- Endometriosis has a devastating effect on women from teenage years to menopause.
- A new National Action Plan for Endometriosis has been launched, prioritising awareness and education, clinical management and care, and research.
- Multidisciplinary management of endometriosis is recommended.
Endometriosis, a disease affecting 1 in 10 Australian women, is rarely spoken about but can have devastating effects on many aspects of a woman’s life. Thankfully, this should change, with the release of a National Action Plan (NAP) for Endometriosis, delivered by Health Minister Greg Hunt last year.
What is Endometriosis?
Endometriosis occurs when cells from the uterine lining (the ‘endometrium’) grow in other parts of the body. It is typically seen inside the pelvis, around the bladder, bowel or uterus, but it can also spread outside the pelvic cavity. During menstruation, this endometrial tissue also bleeds, causing inflammation, scarring and adhesions. The lesions also have a proliferation of nerve endings which become sensitised.
Symptoms of endometriosis can include painful periods, painful sex, chronic pelvic pain, gastrointestinal dysfunction, fatigue, nausea, overactive bladder, migraines, anxiety, and low mood. It is a highly individual disease, with a wide variation of clinical presentations.
Sadly, the average time between onset of symptoms and diagnosis is 7-12 years1. Professor Jason Abbott, gynaecologist and laparoscopic surgeon, suggests that this is partly due to the lack of awareness and ‘taboo’ surrounding endometriosis. Another hurdle to diagnosis is the fact that there is no non-invasive way to diagnose endometriosis, as a firm diagnosis can only be made via laparoscopic surgery. However, symptoms can strongly suggest the diagnosis supported by transvaginal ultrasound, performed by a highly trained operator.
Unfortunately, the cause of endometriosis is not known, and there is no cure. However, it can be effectively managed.
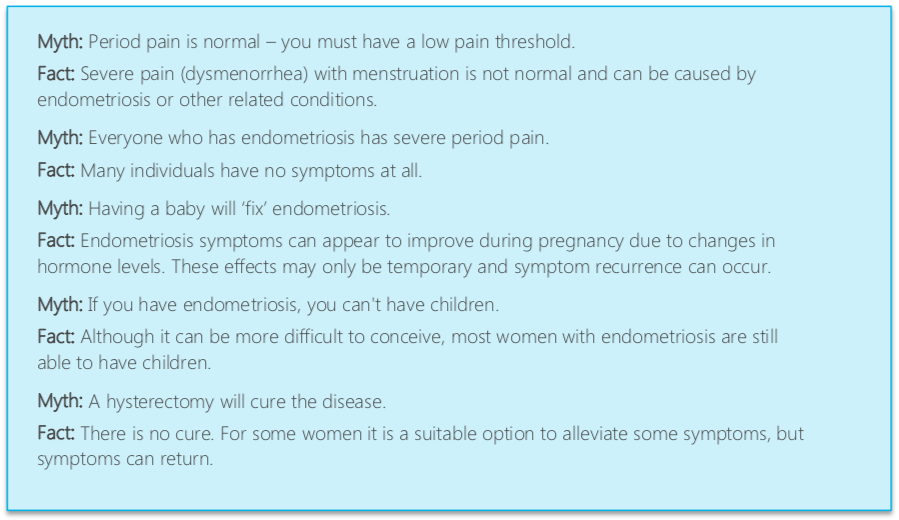
Myths and Facts about Endometriosis
Original image from National Action Plan for Endometriosis, page 1, © Commonwealth of Australia (Department of Health) 2018
National Action Plan For Endometriosis
The NAP provides a glimmer of hope for endometriosis sufferers, addressing three key priority areas:
- Awareness and Education: raising the public profile of endometriosis, and breaking down the ‘taboo’, especially targeted to younger women.
- Clinical Management and Care: improve knowledge and skills of health professionals (including GP’s, specialists, physios and nurses) in optimal management of endometriosis, including treatment of pain with a multidisciplinary approach.
- Research: increasing expenditure on research, with an initial Commonwealth Investment of $2.5 million through the Medical Research Future Fund.
To read the National Action Plan, click here
How To Best Manage Endometriosis
Dr Susan Evans, Gynaecologist and pelvic pain expert, discussed endometriosis on a fascinating episode of SBS Insight that aired late in 2018. She highlighted the devastating impact that endometriosis can have on a teenager, with chronic pain and associated symptoms inhibiting women from developing to their full potential. However, with timely diagnosis and management, Dr Evans is confident we can “change the trajectory of young women’s lives”.
She recommends the following multidisciplinary treatment plan to best manage endometriosis:
1. Stop periods
2. High quality surgical management
3. Lifestyle modification
4. Pelvic floor physiotherapy
5. Dietary changes
6. Address general wellbeing and sleep
To watch this episode on SBS Insight, click here
What Can Pelvic Floor Physios Do To Help?
Painful sex
Typically women with endometriosis will have dyspareunia. Sensitive tissues around the vagina often cause spasm of the pelvic floor muscles around the introitus. The pain leads to withdrawal from intimacy and lack of libido and arousal. Pelvic floor physios teach women how to relax their pelvic floor muscles, use desensitisation techniques such as vaginal trainers to reduce the muscle spasm in response to penetration, and educate women about importance of intimacy, arousal and desire for pain free, enjoyable intercourse.
Chronic Pelvic Pain
Chronic pelvic pain is a complex condition, with endometrial lesions accounting for only one aspect of pain generation for these women. Tight muscles and joints, spasm of the pelvic floor muscles, postural changes, and peripheral and central sensitisation all contribute to the pain experience. Techniques that are helpful include tailored stretching programs, aerobic exercise, strengthening exercises, pelvic floor relaxation and downtraining, and education regarding the science behind the relationship of the brain and nerves to chronic pain.
General wellbeing
‘Self-love’ is very important for these women, and can make a big difference in symptoms. Strategies such as eating well, ensuring they are getting enough good quality sleep, a tailored general exercise routine, and stress management with relaxation or mindfulness techniques can be very effective.
Case Study: Sarah, a 21-year-old with Endometriosis
Sarah was referred to WMHP by a gynaecologist for management of endometriosis-related pelvic pain and dyspareunia. Sarah was diagnosed with endometriosis at age 20 following laparoscopic surgery. Following surgery her pain improved for 6 months, however then returned worse than before. Sarah complained of severe pelvic pain 3 out of every 4 weeks impacting her ability to study, work and exercise, irritable bowels, fatigue, anxiety, and inability to have intercourse due to pain.
Sarah saw another gynaecologist for a second opinion, who started her on a multidisciplinary treatment program, consisting of:
- Insertion of Mirena
- Commencement of oral contraceptive pill
- Daily pain medication: Endep, Naproxen and Panadol osteo
- Referral to pelvic floor physio
- Referral to gastroenterologist
Sarah’s main goals when she first attended physio were to ‘be like a normal 21-year-old’, be able to have sex with her boyfriend, play in the netball team with her girlfriends, and use tampons to go swimming.
Sarah attended physio for 12 months, with a focus on pelvic floor muscle relaxation, gentle internal pelvic floor muscle release, vaginal desensitisation exercises, lots and lots of education about dyspareunia, intimacy, arousal, desire, pain science education and the impact her brain had on her pain, and general lifestyle strategies including daily mindfulness, regular home based yoga via a phone app, and sleep education. Sarah also attended a gastroenterologist and was given dietary modifications and medication.
After 3 months of this team-based treatment approach, Sarah’s pain had reduced significantly, to only moderate period pain for one week per month. She was able to play netball and had used a tampon to go swimming at the beach.
After 12 months, Sarah had weaned off all pain medication and the oral contraceptive pill (Mirena remained in situ). She reported very manageable period pain for 4-5 days per month and found this wasn’t impacting her life at all. She was overjoyed that she was now able to have comfortable, enjoyable sex with her boyfriend, and she felt excited and empowered about her future as a happy, healthy young woman.
Certainly not all women with endometriosis experience this much improvement, but Sarah’s story highlights the possible benefits of a coordinated multidisciplinary team approach.
For more information about endometriosis:
References
1 National Action Plan for Endometriosis, Commonwealth of Australia (Department of Health), 2018,
http://www.health.gov.au/internet/main/publishing.nsf/Content/58AD1EF08402AC9FCA2582D5001A271E/$File/National%20Action%20Plan%20for%20Endometriosis.pdf
March 2019