Highlights From The 23rd Asia-Pacific Prostate Cancer Conference
The 23rd Asia Pacific Prostate Cancer Conference gathered almost 400 of the leading Australian and international Urologists, Oncologists, Pelvic Health Physiotherapists, Prostate Cancer Specialist Nurses, Urology Nurses and other health practitioners in this field together to share the most recent advances in research and treatment and learn about the improved management of prostate cancer. Shan Morrison was part of the organising committee for the conference that developed the Nursing and Allied Health Program.
There was so much to take away from the conference, and here we share the highlights from our perspective as Pelvic Health Physiotherapists involved in the care of Prostate Cancer.
It Takes A Village To Treat Prostate Cancer
The importance of a strong multidisciplinary health care and support team that is patient centred was a strong theme of the conference. The side effects of treatment for prostate cancer have a significant impact of multiple body systems and quality of life. Men and their partners need to understand who can help them along their journey and be empowered to advocate for themselves.
Shan presented on this topic “Applying Best Practice To The Clinical Consultation”, highlighting the importance of the individualised management of post prostatectomy incontinence and using the multidisciplinary team.
Precision Medicine Involves The Right Pelvic Floor Muscle Exercises At The Right Time
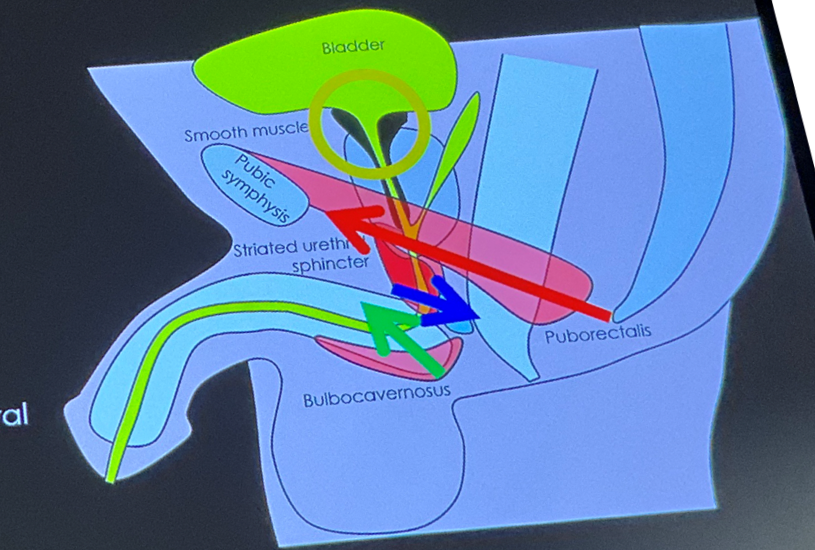
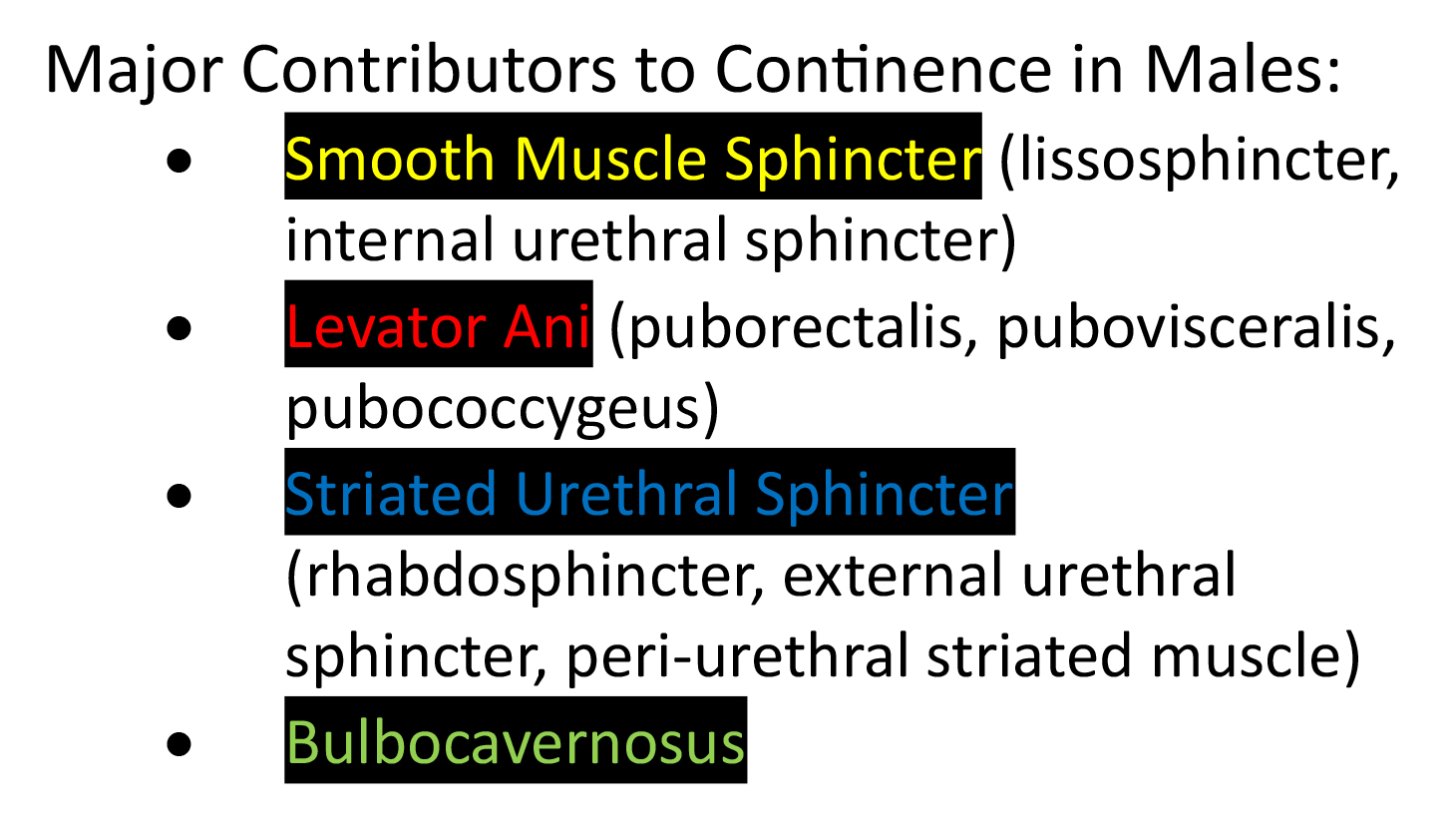
Precision medicine was another theme frequently referred to in relation to the use of diagnostic testing to ensure that the right patient is treated at the right time with the right medicine. This concept of precision medicine also applies to pelvic floor muscle training, where evidence shows that the right pelvic floor muscle contraction with the right cue at the right time is critical to improve outcomes for patients undergoing prostate cancer treatment, particularly prostatectomy.
Professor Paul Hodges, prominent physiotherapist and researcher from The University of Queensland has led ground breaking studies into the use of transperineal ultrasound (TPUS) to assess the function of pelvic floor muscles in men before and after prostate cancer surgery. Shan Morrison, our director at WMHP was also involved in his recent research study, “Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy”1. Their research has led to the following proposed ideal pelvic floor muscle training (PFMT) program of men undergoing prostate surgery:
- Start PFMT pre-operatively, as this helps to condition the striated PFM for their adapted role following prostatectomy.
- Assessment using transperineal ultrasound gives the most accurate assessment and feedback of the function of all of the muscles that need to work together to improve post prostatectomy incontinence.
- The cue used to contract the PFM for those undergoing prostatectomy needs to be specific and biased towards the striated urethral sphincter and avoid contraction of EAS. Optimising the pattern of PFM activity is crucial and should be the first step of PFMT.
- Each man’s pelvic floor exercise program needs to be:
- Functional
- Individualised
- Focused on coordination
- Incorporating low intensity (<10%) hold training for sustained tasks
- Involving high intensity strength and endurance training as the straited muscles need to be strong enough to compensate for the loss of smooth muscle following prostatectomy
- Regularly reassessed and progressed using TPUS for biofeedback
What this really means, is that it is crucial that men undergoing surgery for prostate cancer treatment seek help from a Pelvic Health Physiotherapist before surgery, or if this is not possible, as soon after their catheter is removed as possible. The Pelvic Health Physiotherapist will assess the strength and function of their pelvic floor muscles and prescribe them with the most effective pelvic floor exercise program, designed specifically for them.
Screen For Distress
The need for psychological support for men undergoing treatment for prostate cancer was a strong theme that emerged from the conference. We have previously written about the unmet supportive needs that men report in relation to sexuality, psychological, health system and information issues, and the role that all health professionals can play in supporting the psychological impact of prostate cancer.
The Prostate Cancer Distress Screen is a brief and simple tool that can be used to understand the impact of a prostate cancer diagnosis and the distress that this, along with the side effects of treatment, have on emotional health and wellbeing. The Prostate Cancer Foundation of Australia have released a position statement which includes the following recommendations regarding screening for distress.2
- After the diagnosis of prostate cancer and regularly through treatment and surveillance men who have been diagnosed with prostate cancer should be screened for distress and their psychological and quality of life concerns should be explored.
- Men who have high levels of distress should be further evaluated for anxiety and/or depression and evidence of suicidality.
- Men who have high distress or need for support should be referred to evidence-based intervention matched to their individual needs and preferences for support.
Melissa Martin, one of our experienced Pelvic Health Physiotherapists from WMHP, presented on this topic at the conference. She highlighted the positive impact that WMHP physiotherapists have noticed on wellbeing since implementing this screening tool and understanding that all health professionals involved can provide effective emotional support.
The Impact Of Sexual Dysfunction Takes A Toll
Dr Chris Nelson is both a clinician and a researcher and is the head of the Psychiatry / Psychology Department at Memorial Sloan Kettering Cancer Centre in New York. He has a focus on understanding and supporting men and their partners to optimise intimacy and addressing the psychological problems that arise with incontinence and sexual dysfunction following prostate cancer treatment. We are choosing to use the term sexual dysfunction here, which encompasses both erectile dysfunction and the psychosocial implications that this causes including a loss of libido, arousal and intimacy.
It is well established that sexual dysfunction is associated with depression & distress, which often leads to withdrawal from social and intimate situations. Dr Nelson and his research team have found that the level of bother experienced about sexual dysfunction doesn’t reduce over time (ie men simply don’t just ‘get used to it’ as times goes on)3.
Through his qualitative research, (Nelson et al) found the following themes that men reported when asked about their experiences with sexual dysfunction post prostatectomy and the treatment options offered to them:
- frustration with the lack of information about post-surgery sexual dysfunction and a desire to have more information about the side effects of treatment prior to treatment starting, including realistic expectations without an ‘over-promise’ of recovery of erectile function
- negative emotional impact of sexual dysfunction and avoidance of sexual situations including their sense of deep disappointment and distress
- negative emotional experience with penile injections and barriers leading to avoidance; where men who focused on the longer term benefits rather than negative short term experiences maintained the treatment for longer
- the benefit of focusing on the long-term advantage of rehabilitation versus short-term anxiety
- using humour to help cope
- the benefit of support from partners and peers.
Men Avoid & Drop Out of Erectile Dysfunction Treatment
Studies have shown that many men will drop out of treatment for ED, reporting a 50% drop out rate of PDE5i users and only 10% of men using injections at a rate suggested for rehabilitation3.
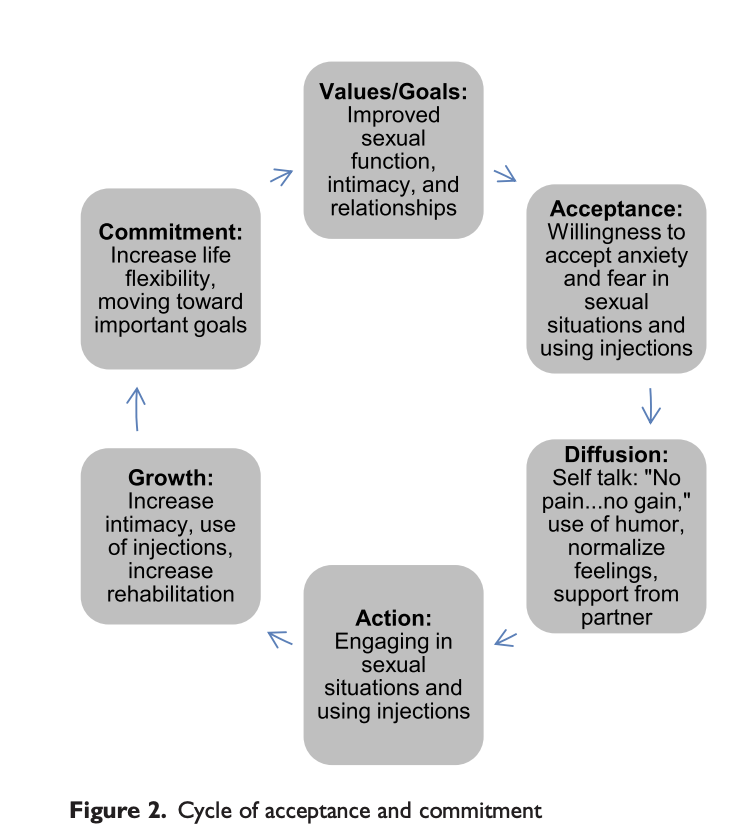
Dr Nelson’s research group have suggested that an Acceptance Commitment Therapy (ACT) framework can be used to assist men with changing the cycle of avoidance of the treatments available for ED into a cycle of commitment. Through defining important values, accepting and acknowledging the emotional distress caused by the treatment, gradually exposing them to the activity whilst providing emotional support can help commitment to a regimen that may have a more favourable outcome in terms of erectile function and emotional wellbeing.
As such, ACT may serve as an important conceptual underpinning of a psychological intervention to help men reduce avoidance and adhere to a penile rehabilitation program following radical prostatectomy3.
As physiotherapists, we find that as men’s incontinence improves, their attention will turn to addressing their ED. They may have been provided with instructions from their Urologist, Urology Nurse or Prostate Cancer Specialist Nurse about PDE5i inhibitors, vacuum pump or injections. We certainly see men in this avoidance cycle and find using the cycle of acceptance and commitment above to be a helpful communication tool to increase engagement with these therapies.
Prostate Cancer Survivorship Essentials Framework: A Resource To Support Men
In response to the research revealing the need for more psychological support for men with prostate cancer, a group of Australian based Urologists, Psychologists and specialists in Prostate Cancer developed the Prostate Cancer Survivorship Essentials Framework.
They developed a plan that includes intervention options and support for survivors of prostate cancer. They acknowledge that any person who has had a cancer diagnosis is considered to be a survivor. Survivorship care means having a plan to look after their wellbeing now and for any changes that might happen in the future.
The plan includes 6 areas to consider, which includes:
- Personal Agency: understanding what support is available to, what to do to help themselves and what others can offer.
- Shared Management: being involved in decision making with their whole health care team.
- Vigilance: their health care team keeping on top of the control of the cancer, the management of side effects and also checking in on emotional and social wellbeing.
- Evidence-based survivorship interventions: ensuring that treatment and management is based on up to date research and evidence.
- Care Coordination: the health care team communicating and working together to give them the best care.
- Heath Promotion and Advocacy: having the most up to date and accurate information provided.
This survivorship framework has been developed into a Wellness Plan, that can be used to summarise the information about diagnosis, treatment and progress. This plan can be downloaded from the Prostate Cancer Foundation of Australia.
References
1 Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H et al. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. Urologic Oncology, Seminars and Original Investigations. 2020;38: 354−371
2 https://www.pcfa.org.au/media/789913/uts-impacct-positionstatement_online.pdf
3 Nelson CJ, Lacey S, Kenowitz J, Pessin H, Shuk E and Mulha JP. Men’s experience with penile rehabilitation following radical prostatectomy: a qualitative study with the goal of informing a therapeutic intervention. Psycho-Oncology. 2015; DOI: 10.1002/pon.3771
September 2023