What Is Pregnancy Related Pelvic Girdle Pain (PPGP)?
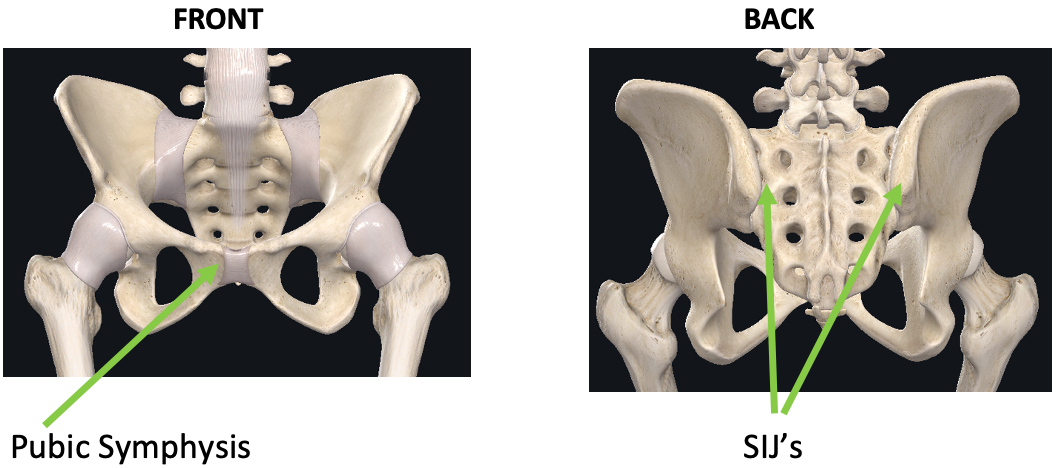
PPGP is pain in the buttock area or sacro-iliac joints (SIJs), the area of the back where the spine joins the pelvis and/or the pubic symphysis (where the pubic bones join together at the front). Sometimes the pain may also be felt in the back of the thigh. People with PPGP often have pain and difficulties with standing, walking, sitting and changing positions (eg rolling over in bed, getting up from a chair). It can have a significant impact on quality of life, ability to work throughout pregnancy and can cause substantial disability.
How Common Is PPGP?
PPGP may occur in up to 72% of pregnant women, with almost 50% reporting symptoms earlier than 20 weeks into their pregnancy and 20% reporting severe symptoms from 20–30 weeks.
Are PPGP and Pelvic Instability The Same Thing?
PPGP is often misdiagnosed as pelvic instability. The pubic symphysis and the SIJ’s are very stable joints, with very little movement occurring. The term ‘Pelvic Instability’ is an outdated term and an incorrect diagnosis for most people with PPGP.
Pregnancy related Pelvic Girdle Pain is NOT due to pelvic instability.
Is PPGP Caused By The Pregnancy Hormone Relaxin?
All pregnant people experience hormonal changes to accommodate the demands of pregnancy. These changes can lead to increased tissue sensitivity, flexibility and inflammatory processes in the body, with the pelvis remaining stable throughout pregnancy.
There is no evidence that supports the hormone Relaxin as the cause of PPGP in pregnancy.
Consider this: if pregnancy hormones were the main factors contributing to pain, all pregnant women would have PPGP, which they don’t!
What Causes PPGP?
Recent research uncovered surprising risk factors associated with PPGP:
- Previous trauma – including trauma associated with miscarriages, fertility treatments, pregnancy, previous births and the postpartum period.
- Psychosocial factors (including thoughts, feelings and behaviours)
- Changes to the nervous system which may increase sensitivity
- High body mass index
- Smoking
- Confidence or belief in improvement.
Factors that are NOT associated with PPGP:
- Hormones ie Relaxin
- Posture
- Exercise and moving (in fact, it is safe and beneficial to move and exercise in pregnancy, even when experiencing PPGP)
- Breast feeding
- Vaginal birth
What Can be done to help PPGP?
Many people are told that PPGP is a normal part of pregnancy and that they should just put up with it until the baby is born. Not only is this advice not helpful, it is untrue! There are many strategies that can help PPGP, often starting with a Pelvic Health Physiotherapy assessment.
This involves taking a thorough history to understand the contributing factors and a physical examination to assess the muscles, ligaments and nerves around the pelvis. Physiotherapists commonly find muscle guarding and tension, which can lead to further discomfort, increased sensitivity and fear of movement. Assessment may also involve exploring thoughts and beliefs regarding pain and its impact.
An individualised treatment plan is designed collaboratively based on symptoms, lifestyle and goals, with the aim for PPGP to be self-manageable. Some of the treatment options may include:
- Modification and pacing of activity levels
- Education to help understand PPGP and why it happens
- A movement program incorporating various cardio-vascular, stretches, strengthening or relaxation exercises (eg of abdominal or pelvic floor muscles) and mindful movement
- A pregnancy belt or tape can improve the feeling of support and reduce muscle guarding to allow to more freedom of movement
- Hands on treatment
- Strategies to improve sleep
- Meditation or mindfulness to reduce nervous system sensitivity
- Healthy eating
- Cease smoking
Exercise has been shown to help prevent & reduce PPGP in pregnancy
Does PPGP Continue After Childbirth?
For most people, PPGP settles once the baby is born. For some, pain may continue and require further treatment and exercise to improve.
An assessment with a Pelvic Health Physiotherapist is recommended 3-6 weeks after birth. The focus of a postnatal physiotherapy program will be on returning to normal daily activities, restoring pelvic floor and abdominal muscle function and safe return to exercise.
Will PPGP Return In Another Pregnancy?
With appropriate assessment and management, PPGP can be successfully treated and prevented from recurring in a subsequent pregnancy.
Want To Learn More?
In 2022, a group of Canadian researchers and clinicians published a wonderful infographic that reframes beliefs about PPGP for patients and healthcare professionals. They acknowledge that there is no evidence to support many commonly held incorrect beliefs regarding PPGP, which can contribute to PPGP worsening or continuing.
At WMHP, we wholeheartedly believe in the conclusions shared by this group of researchers:
Early intervention for PPGP is essential to help pregnant people make sense of their pain experience, believe in the possibility of change and adopt positive lifestyle habits throughout their pregnancy for improved health and birth outcomes.